You have encountered a formidable challenge if you or someone you know has experienced a stroke. The immediate aftermath often brings a sense of profound loss, as neurological functions that were once effortless become difficult or impossible. Yet, within the intricate architecture of your brain lies an astonishing capacity for change and adaptation, a phenomenon known as neuroplasticity. This article will guide you through understanding how your brain can rewire itself after injury, offering insights into the mechanisms and strategies that can unlock the remarkable potential for stroke recovery.
When a stroke occurs, it deprives a portion of your brain of vital oxygen and nutrients, leading to the death of brain cells in the affected area. This damage can manifest in a wide range of deficits, impacting your motor control, speech, sensation, cognition, and emotional regulation. The specific symptoms you experience depend on the location and extent of the brain tissue affected. Imagine your brain as a complex city, with various districts responsible for different functions. A stroke is akin to a sudden power outage or a major road closure in one of these critical districts.
Ischemic vs. Hemorrhagic Strokes
It’s important to differentiate between the two main types of stroke, as their underlying causes and initial treatments vary.
- Ischemic Stroke: This is the most common type, accounting for approximately 87% of all strokes. It occurs when a blood clot blocks a blood vessel supplying blood to your brain. Think of it as a clogged pipeline preventing essential resources from reaching their destination.
- Hemorrhagic Stroke: This less common but often more severe type of stroke occurs when a blood vessel in your brain ruptures, bleeding into the surrounding brain tissue. This can be compared to a burst pipe flooding an area, causing damage not only from the deprivation of resources but also from the pressure and toxicity of the leaked fluid.
Primary vs. Secondary Brain Damage
The damage inflicted by a stroke is not always immediate and singular.
- Primary Damage: This refers to the direct brain cell death (infarction) in the area immediately deprived of blood flow. This is the immediate impact, the initial blow.
- Secondary Damage: This occurs in the hours, days, and even weeks following the initial stroke. It involves processes such as inflammation, swelling (edema), and the release of neurotoxic chemicals that can harm surrounding, initially unaffected brain tissue. Understanding this secondary damage is crucial, as therapeutic interventions often aim to mitigate its effects and protect the “at-risk” tissue, often referred to as the penumbra.
Functional Deficits Post-Stroke
The range of impairments you might experience after a stroke is vast and highly individualized.
- Motor Deficits: You might experience weakness (paresis) or paralysis (plegia) on one side of your body, difficulty with coordination, balance issues, or problems with fine motor skills. Tasks like tying your shoelaces or holding a pen can become incredibly challenging.
- Speech and Language Deficits: Aphasia, a disorder affecting your ability to understand or produce language, is common. This can range from difficulty finding the right words to complete inability to speak or comprehend. Imagine trying to communicate when your internal dictionary has been scrambled.
- Sensory Deficits: You might experience numbness, tingling, or altered sensation on one side of your body. Proprioception, your sense of body position, can also be affected, making it difficult to know where your limbs are without looking.
- Cognitive Deficits: This can include problems with memory, attention, executive functions (planning, problem-solving), and spatial awareness. Everyday tasks requiring sequential thought or multi-tasking can become overwhelming.
- Emotional and Psychological Deficits: Stroke can also lead to depression, anxiety, mood swings, and emotional lability (sudden, unprovoked emotional outbursts). The psychological impact of losing previously held abilities is significant and requires careful consideration.
Neuroplasticity plays a crucial role in stroke recovery for adults, as it refers to the brain’s ability to reorganize itself by forming new neural connections. This remarkable capacity allows individuals to regain lost functions and adapt to changes after a stroke. For a deeper understanding of how neuroplasticity can aid in rehabilitation, you can read a related article on this topic at Unplugged Psychology, which explores various therapeutic approaches and exercises that harness the brain’s adaptability to enhance recovery outcomes.
The Principle of Neuroplasticity: Your Brain’s Remarkable Adaptability
At the heart of stroke recovery lies the extraordinary capacity of your brain to reorganize itself. Neuroplasticity, often referred to as brain plasticity, is the lifelong ability of your brain to form new neural connections, reorganize existing ones, and even generate new neurons. It’s the brain’s built-in mechanism for learning, memory, and adaptation. After a stroke, neuroplasticity becomes your primary ally, the engine driving the recovery process. Think of it as your brain’s inherent ability to reroute traffic around a major road closure, finding alternative paths and even building new ones to maintain essential services.
Synaptic Plasticity: Strengthening and Weakening Connections
One of the most fundamental mechanisms of neuroplasticity occurs at the level of the synapse, the junction between two neurons.
- Long-Term Potentiation (LTP): This is a persistent strengthening of synaptic efficacy that occurs after high-frequency stimulation. In simpler terms, when two neurons repeatedly communicate, their connection becomes stronger, making future communication more efficient. This is how your brain learns and forms memories; it’s also how new motor skills are consolidated during rehabilitation.
- Long-Term Depression (LTD): Conversely, LTD is a persistent weakening of synaptic efficacy, often occurring after low-frequency stimulation. This process is crucial for “unlearning” ineffective or unwanted connections and for refining neural circuits. Your brain constantly prunes unused or inefficient pathways, making room for more useful ones.
Structural Plasticity: Changes in Brain Anatomy
Neuroplasticity is not just about strengthening or weakening existing connections; it also involves more profound structural changes.
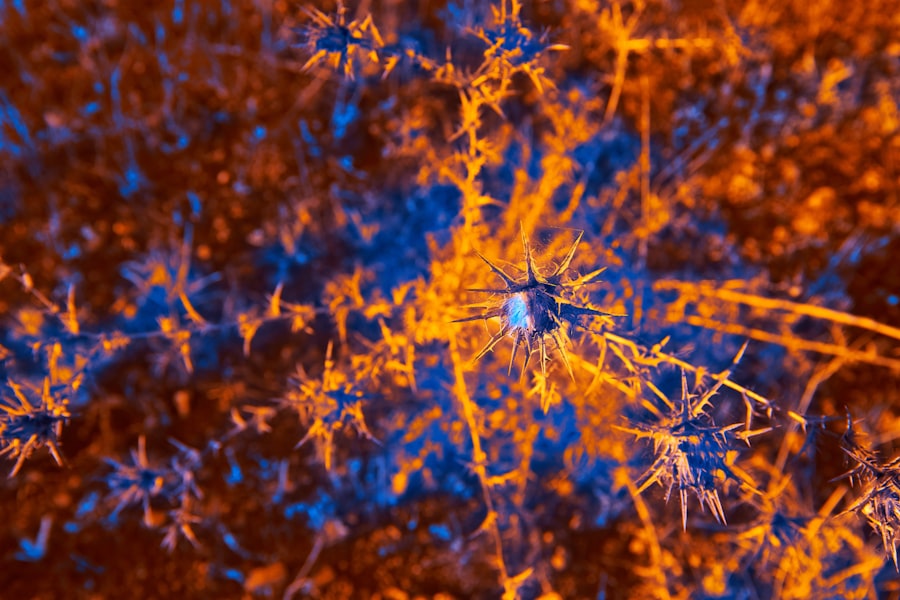
- Axonal Sprouting: After an injury, surviving neurons can grow new axonal branches to form new connections with other neurons. Imagine existing telephone wires extending new lines to reach previously unconnected houses.
- Dendritic Branching: Dendrites, the tree-like structures that receive signals from other neurons, can grow new branches and expand their receptive fields, increasing the number of connections a neuron can make.
- Neurogenesis: While once thought to be limited to development, research has shown that new neurons can be generated in certain areas of the adult brain, particularly in the hippocampus (involved in memory) and the subventricular zone (which can migrate to other areas). While the extent of its contribution to stroke recovery is still being investigated, it represents another fascinating avenue of brain regeneration.
Functional Reorganization: Shifting Responsibilities
Perhaps the most dramatic aspect of neuroplasticity in stroke recovery is functional reorganization. When an area of your brain is damaged, other, often adjacent or even remote, brain regions can take over the functions that were once performed by the injured area. This is like a city district losing its bank, and a neighboring district expanding its financial services to compensate for the loss. This can involve:
- Recruitment of ipsilateral pathways: The opposite hemisphere of your brain, which normally controls the other side of your body, can sometimes contribute to motor recovery on the affected side.
- Activation of redundant pathways: Your brain often has multiple pathways for performing certain functions. After a stroke, previously dormant or less dominant pathways can be recruited and strengthened.
- Cortical remapping: The cortical representation of body parts can change. For example, if your hand movement area is damaged, the representation of your shoulder or elbow might expand, or even the unaffected hand’s representation can increase.
The Critical Role of Rehabilitation and Targeted Intervention
Understanding neuroplasticity is only the first step. The true power of this phenomenon is harnessed through active and targeted rehabilitation. Your brain needs specific stimuli and challenges to drive its rewiring process. Think of rehabilitation as providing the blueprint and the necessary tools for your brain to reconstruct its damaged pathways.
Intensity and Repetition: The Pillars of Recovery
Just as you wouldn’t expect to build a strong muscle by lifting weights only occasionally, your brain requires consistent and repetitive stimulation to reorganize effectively.
- High-Intensity Training: Engaging in tasks that challenge your limits, even slightly, stimulates greater neuroplastic changes. It pushes your brain to adapt and strengthen new connections.
- Task-Specific Practice: Focusing on specific movements or functions you want to regain, rather than just general exercises, is crucial. If you want to improve your grip, perform exercises that directly involve gripping objects. This ensures that the neural pathways relevant to that specific task are being activated and reinforced.
###Constraint-Induced Movement Therapy (CIMT): Overcoming Learned Non-Use
CIMT is a powerful rehabilitation technique that directly leverages neuroplasticity. It involves restricting the movement of your unaffected limb, forcing you to use your affected limb for many hours a day.
- Addressing Learned Non-Use: After a stroke, you might naturally gravitate towards using your unaffected limb because it’s easier. Over time, your brain can “learn” that the affected limb is useless, even if some function remains. CIMT systematically breaks this cycle.
- Forced Use and Cortical Reorganization: By forcing the use of the affected limb, CIMT drives intense activation of the motor pathways associated with that limb, promoting significant cortical reorganization and functional recovery. It’s like gently pushing a shy child onto a playground until they discover the joy of playing with others.
Robotics and Virtual Reality: Innovative Tools for Engagement
Technological advancements are revolutionizing stroke rehabilitation by providing engaging and measurable interventions.
- Robotic-Assisted Therapy: Robots can provide repetitive, high-intensity training that might be difficult for therapists to sustain. They can also offer precise feedback and assist with movements, gradually reducing assistance as your function improves.
- Virtual Reality (VR): VR environments can immerse you in simulated tasks that are motivating and challenging. This allows for safe practice of real-world activities, instant feedback, and the ability to track your progress in a gamified way. Imagine practicing grocery shopping or navigating a busy street within a safe, controlled digital environment.
The Importance of Holistic Care and Long-Term Engagement

Stroke recovery is not a sprint; it is an marathon. While the initial weeks and months often see the most dramatic improvements, your brain’s capacity for neuroplasticity continues for years, even decades, after a stroke. Embracing a holistic approach to your health and maintaining long-term engagement with activities that promote brain health are vital.
Cognitive Rehabilitation: Rewiring Your Thinking
Beyond motor and language recovery, addressing cognitive deficits is equally important.
- Memory Training: Strategies like spaced repetition, chunking information, and using mnemonic devices can help your brain reconstruct or find alternative routes to memory retrieval.
- Attention Training: Exercises that require sustained focus, selective attention, and dividing attention can strengthen the neural networks involved in these processes.
- Executive Function Training: Engaging in problem-solving tasks, planning activities, and organizational strategies can help your brain regain its ability to regulate and direct complex behaviors.
Lifestyle Factors: Fueling Your Brain’s Recovery
Your overall health significantly influences your brain’s ability to heal and reorganize.
- Physical Activity: Regular exercise, even moderate activity, promotes blood flow to your brain, stimulates the release of growth factors, and reduces inflammation, all of which support neuroplasticity.
- Nutrition: A balanced diet rich in antioxidants, omega-3 fatty acids, and essential vitamins and minerals provides the building blocks for healthy brain function. Avoid processed foods, excessive sugar, and unhealthy fats.
- Sleep: Quality sleep is crucial for memory consolidation, cellular repair, and brain detoxification. Prioritize consistent sleep patterns.
- Stress Management: Chronic stress can impair neuroplasticity. Techniques such as mindfulness, meditation, and deep breathing can help mitigate stress and protect your brain.
Social Engagement and Emotional Support: The Human Connection
Recovering from a stroke can be an isolating experience. Maintaining strong social connections and seeking emotional support are essential for your well-being and can indirectly support brain recovery.
- Support Groups: Connecting with others who have undergone similar experiences can provide a sense of community, shared strategies, and emotional validation.
- Family and Friends: A supportive network of loved ones can offer encouragement, practical assistance, and motivation to continue with rehabilitation.
- Mental Health Professionals: Therapists and counselors can help you navigate the emotional challenges of stroke recovery, such as depression, anxiety, and grief.
Neuroplasticity plays a crucial role in stroke recovery for adults, as it allows the brain to reorganize and form new connections in response to injury. Recent studies have shown that engaging in targeted therapies can significantly enhance this natural healing process. For those interested in exploring this topic further, a related article discusses various rehabilitation strategies that leverage neuroplasticity to improve outcomes for stroke survivors. You can read more about these innovative approaches in the article found here.
The Future of Stroke Recovery: Emerging Therapies and Research
| Metric | Description | Typical Range/Value | Relevance to Stroke Recovery |
|---|---|---|---|
| Neurogenesis Rate | Rate of new neuron formation in the brain | Approximately 700 new neurons/day in hippocampus | Supports formation of new neural pathways post-stroke |
| Synaptic Plasticity | Ability of synapses to strengthen or weaken over time | Long-term potentiation (LTP) magnitude varies by region | Enhances relearning of motor and cognitive functions |
| Cortical Map Reorganization | Changes in brain area representations after injury | Up to 20-30% reorganization observed in motor cortex | Enables compensation for lost functions by adjacent areas |
| Functional Connectivity | Strength of communication between brain regions | Increased connectivity in perilesional areas post-therapy | Correlates with improved motor and cognitive recovery |
| Time Window for Plasticity | Period post-stroke when brain plasticity is heightened | Typically 3-6 months, with some plasticity up to 1 year | Critical period for intensive rehabilitation interventions |
| Motor Function Improvement | Measured by scales like Fugl-Meyer Assessment (FMA) | Average improvement: 10-20 points in subacute phase | Indicator of successful neuroplastic changes |
| Cognitive Recovery Metrics | Tests such as MoCA or MMSE scores post-stroke | Improvement of 2-5 points within 6 months | Reflects neuroplasticity in cognitive domains |
The field of stroke recovery is dynamic, with ongoing research continually uncovering new insights and developing innovative therapies. You are living in an exciting era where our understanding of the brain’s healing potential is rapidly expanding.
Pharmacological Interventions: Enhancing Neuroplasticity
Researchers are exploring drugs that can directly enhance neuroplasticity or reduce secondary brain damage.
- Neurotrophic Factors: These are proteins that promote the growth, survival, and differentiation of neurons. Administering such factors could potentially boost the brain’s natural repair mechanisms.
- Modulators of Synaptic Plasticity: Drugs that specifically target and enhance LTP or suppress LTD are being investigated to optimize learning and memory formation during rehabilitation.
Brain Stimulation Techniques: Directing Brain Activity
Non-invasive brain stimulation methods offer promising avenues for modulating brain activity and promoting recovery.
- Transcranial Magnetic Stimulation (TMS): This technique uses magnetic pulses to stimulate specific areas of your brain. It can be used to excite underactive areas or inhibit overactive ones, thereby rebalancing brain circuitries.
- Transcranial Direct Current Stimulation (tDCS): tDCS applies a weak electrical current to your scalp, which can modulate neuronal excitability. It’s often used in conjunction with rehabilitation exercises to enhance their effectiveness.
Stem Cell Therapy: Repairing and Replacing Damaged Cells
While still largely experimental, the use of stem cells holds significant promise for stroke recovery.
- Cell Replacement: Stem cells could potentially replace neurons and other brain cells lost due to the stroke.
- Neuroprotection and Trophic Support: Even without direct cell replacement, stem cells can release growth factors and anti-inflammatory molecules that protect surviving brain tissue and create a more favorable environment for neuroplasticity.
In conclusion, confronting the aftermath of a stroke is an immense challenge, but your brain possesses an inherent capacity for adaptation and repair. By understanding the principles of neuroplasticity and actively engaging in targeted, intensive, and long-term rehabilitation, you can unlock this remarkable potential. The journey of stroke recovery is a testament to the brain’s resilience, its ability to reroute, rebuild, and re-learn. Embrace the process, advocate for your care, and believe in your brain’s extraordinary ability to heal.
FAQs
What is neuroplasticity and how does it relate to stroke recovery?
Neuroplasticity is the brain’s ability to reorganize itself by forming new neural connections throughout life. After a stroke, neuroplasticity allows the brain to compensate for damaged areas by rerouting functions to healthy regions, which is essential for recovery of lost skills and functions.
How does neuroplasticity aid in regaining motor skills after a stroke?
Neuroplasticity helps in regaining motor skills by enabling the brain to adapt and create new pathways that control movement. Through repetitive practice and rehabilitation exercises, patients can strengthen these new connections, improving coordination, strength, and control in affected limbs.
What types of therapies utilize neuroplasticity for stroke recovery?
Therapies such as physical therapy, occupational therapy, speech therapy, constraint-induced movement therapy, and task-specific training leverage neuroplasticity. These therapies focus on repetitive, targeted activities that encourage the brain to rewire and restore lost functions.
How long does neuroplasticity-driven recovery typically take after a stroke?
Recovery timelines vary widely depending on stroke severity, location, and individual factors. Neuroplasticity can continue for months or even years post-stroke, but the most significant improvements often occur within the first six months. Consistent rehabilitation can enhance and prolong recovery.
Can neuroplasticity be enhanced to improve stroke recovery outcomes?
Yes, neuroplasticity can be enhanced through various methods including intensive rehabilitation, aerobic exercise, brain stimulation techniques (like transcranial magnetic stimulation), and maintaining a healthy lifestyle with proper nutrition and sleep. These approaches help optimize brain function and recovery potential.