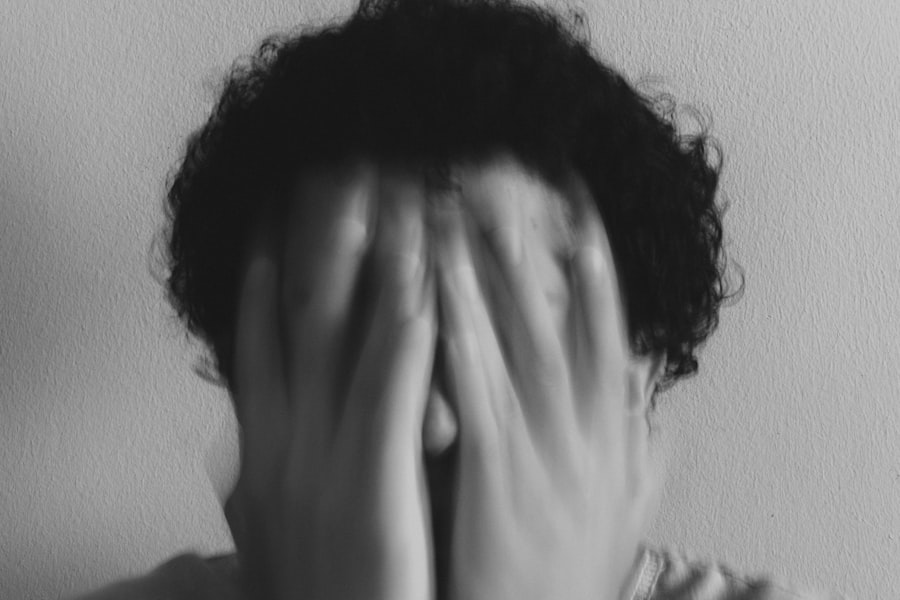
Depersonalization and Derealization Disorder (DPDR) is a complex mental health condition characterized by persistent feelings of detachment from oneself or the surrounding environment. You may find yourself feeling as though you are an outside observer of your thoughts, emotions, or body, leading to a sense of unreality. This disorder can manifest in two primary forms: depersonalization, where you feel disconnected from your own self, and derealization, where the world around you seems distorted or unreal.
These experiences can be disorienting and frightening, often leaving you questioning your own identity and the nature of reality itself. The disorder is not merely a fleeting feeling; it can become chronic and significantly impact your daily life. Many individuals with DPDR report that these episodes can be triggered by stress, anxiety, or trauma, making it essential to understand the nuances of this condition.
While it can occur in isolation, it often coexists with other mental health issues, complicating the overall picture. Understanding DPDR is crucial for recognizing its symptoms and seeking appropriate help.
Key Takeaways
- Depersonalization and Derealization Disorder is a mental health condition characterized by feeling detached from oneself and the surrounding environment.
- Symptoms of Depersonalization and Derealization Disorder include feeling like an outside observer of one’s thoughts and actions, and experiencing a sense of unreality or detachment from the world.
- The causes of Depersonalization and Derealization Disorder are not fully understood, but may be related to trauma, stress, or other mental health conditions.
- Diagnosis of Depersonalization and Derealization Disorder involves a thorough evaluation of symptoms and ruling out other potential causes.
- Treatment options for Depersonalization and Derealization Disorder may include therapy, medication, and lifestyle changes to manage symptoms and improve quality of life.
Symptoms of Depersonalization and Derealization Disorder
The symptoms of Depersonalization and Derealization Disorder can vary widely from person to person, but they generally revolve around the core experiences of detachment and unreality. You might experience a sense of being disconnected from your thoughts or feelings, as if you are watching yourself from a distance. This can lead to feelings of numbness or emotional flatness, making it difficult to engage fully with your life.
You may also notice that your perception of time feels altered; moments may seem to stretch or compress in ways that are disconcerting. In addition to these core symptoms, you might experience physical sensations that contribute to the feeling of unreality. For instance, your body may feel strange or unfamiliar, as if it doesn’t belong to you.
You may also perceive your surroundings as dreamlike or foggy, where familiar places seem foreign or distorted. These experiences can be distressing and may lead to increased anxiety or panic attacks, further complicating your emotional landscape. Recognizing these symptoms is the first step toward understanding your experiences and seeking help.
Causes of Depersonalization and Derealization Disorder

The exact causes of Depersonalization and Derealization Disorder remain somewhat elusive, but research suggests that a combination of biological, psychological, and environmental factors may play a role. You might find that high levels of stress or trauma are significant contributors to the onset of DPDR. For instance, experiencing a traumatic event—such as an accident, abuse, or loss—can trigger feelings of depersonalization as a coping mechanism.
Your mind may create a sense of detachment to protect you from overwhelming emotions associated with the trauma. Additionally, certain personality traits or predispositions may make you more susceptible to developing DPDR. Individuals who are prone to anxiety or have a history of mood disorders may be at higher risk.
Neurobiological factors, such as imbalances in neurotransmitters or alterations in brain function, could also contribute to the disorder. Understanding these potential causes can help you make sense of your experiences and guide you toward effective treatment options.
Diagnosis of Depersonalization and Derealization Disorder
| Diagnosis of Depersonalization and Derealization Disorder | |
|---|---|
| Prevalence | 1-2% of the population |
| Age of Onset | Usually in adolescence or early adulthood |
| Duration | Episodes can last for hours, days, months, or even years |
| Symptoms | Feelings of detachment from oneself or the environment, altered perception of reality, emotional numbness |
| Diagnostic Criteria | Presence of persistent or recurrent episodes of depersonalization, derealization, or both |
| Treatment | Therapy (e.g., cognitive-behavioral therapy), medication (e.g., antidepressants) |
Diagnosing Depersonalization and Derealization Disorder typically involves a comprehensive evaluation by a mental health professional. You may undergo a series of interviews and assessments designed to explore your symptoms in depth. The clinician will likely ask about the frequency and duration of your experiences, as well as any potential triggers that may exacerbate your feelings of detachment or unreality.
It’s essential to provide as much detail as possible during this process to ensure an accurate diagnosis. In some cases, your clinician may also rule out other mental health conditions that could mimic the symptoms of DPDR. For example, anxiety disorders, mood disorders, and certain psychotic disorders can present with similar feelings of detachment or altered perception.
A thorough assessment will help distinguish DPDR from these other conditions, allowing for a more targeted approach to treatment. Understanding the diagnostic process can empower you to seek help and advocate for your mental health needs.
Treatment Options for Depersonalization and Derealization Disorder
When it comes to treating Depersonalization and Derealization Disorder, a multifaceted approach is often most effective. You may benefit from psychotherapy, particularly cognitive-behavioral therapy (CBT), which focuses on identifying and changing negative thought patterns associated with your experiences. Through therapy, you can learn coping strategies to manage symptoms and reduce feelings of detachment.
Additionally, mindfulness techniques can help ground you in the present moment, fostering a greater connection to yourself and your surroundings. In some cases, medication may be prescribed to address underlying anxiety or depression that could be contributing to your symptoms. Antidepressants or anti-anxiety medications might be considered based on your specific needs.
It’s important to work closely with your healthcare provider to determine the best course of action for your situation.
Understanding the Impact of Depersonalization and Derealization Disorder on Daily Life
Living with Depersonalization and Derealization Disorder can profoundly affect various aspects of your daily life. You may find it challenging to engage in social situations or maintain relationships due to feelings of disconnection from yourself and others. This sense of alienation can lead to isolation, making it difficult for you to reach out for support or connect with loved ones.
The emotional toll can be significant, often resulting in increased anxiety or depression. Moreover, everyday tasks may become daunting when you struggle with feelings of unreality. Activities that once brought joy might feel meaningless or overwhelming.
You may find it hard to concentrate at work or school, impacting your performance and overall quality of life. Understanding how DPDR affects your daily functioning is crucial for developing effective coping strategies and seeking appropriate support.
Co-occurring Disorders and Depersonalization and Derealization Disorder
Depersonalization and Derealization Disorder often coexists with other mental health conditions, complicating the overall clinical picture. You might find that anxiety disorders, depression, post-traumatic stress disorder (PTSD), or substance use disorders frequently accompany DPDR. These co-occurring conditions can exacerbate symptoms and make treatment more challenging.
For instance, if you struggle with anxiety alongside DPDR, the heightened stress may intensify feelings of detachment. Recognizing the presence of co-occurring disorders is essential for effective treatment planning. A comprehensive approach that addresses all aspects of your mental health can lead to better outcomes.
Your mental health professional will likely consider these factors when developing a treatment plan tailored to your unique needs.
The Relationship Between Trauma and Depersonalization and Derealization Disorder
Trauma plays a significant role in the development of Depersonalization and Derealization Disorder for many individuals. You may find that past traumatic experiences—whether acute or chronic—can trigger episodes of depersonalization as a protective mechanism against overwhelming emotions. The mind often resorts to dissociation as a way to cope with distressing memories or feelings associated with trauma.
Understanding this relationship between trauma and DPDR can be empowering for you as you navigate your healing journey. By addressing underlying trauma through therapy or other interventions, you may find relief from symptoms and a greater sense of connection to yourself and the world around you. Trauma-informed care is essential in treating DPDR effectively.
How Depersonalization and Derealization Disorder is Different from Other Mental Health Disorders
While Depersonalization and Derealization Disorder shares some similarities with other mental health conditions, it possesses unique characteristics that set it apart. Unlike anxiety disorders or mood disorders that primarily focus on emotional regulation, DPDR centers around experiences of detachment from self and reality. You might notice that while anxiety manifests through excessive worry or fear, DPDR presents as a profound sense of disconnection.
Additionally, DPDR is often episodic in nature; you may experience periods of intense detachment followed by times when you feel more grounded in reality. This fluctuation distinguishes it from chronic conditions like schizophrenia or bipolar disorder, where symptoms tend to be more persistent or pervasive. Understanding these differences can help you articulate your experiences more clearly when seeking support.
Coping Strategies for Individuals with Depersonalization and Derealization Disorder
Developing effective coping strategies is crucial for managing the symptoms of Depersonalization and Derealization Disorder in your daily life. Grounding techniques can be particularly helpful; these practices encourage you to reconnect with the present moment through sensory experiences. For instance, focusing on physical sensations—such as feeling the texture of an object or listening to ambient sounds—can help anchor you in reality when feelings of detachment arise.
Additionally, maintaining a routine can provide structure and stability amidst the chaos of DPDR symptoms. Engaging in regular physical activity, practicing mindfulness meditation, or journaling about your experiences can foster a greater sense of control over your thoughts and emotions. Experimenting with different coping strategies will allow you to discover what works best for you on your journey toward healing.
Seeking Support for Depersonalization and Derealization Disorder
Seeking support is an essential step in managing Depersonalization and Derealization Disorder effectively. You don’t have to navigate this journey alone; reaching out to mental health professionals who specialize in dissociative disorders can provide valuable guidance and understanding. Therapy offers a safe space for you to explore your experiences without judgment while equipping you with tools to cope with symptoms.
Additionally, connecting with support groups—either in-person or online—can foster a sense of community among individuals who share similar experiences. Hearing others’ stories can help normalize your feelings and provide insights into effective coping strategies. Remember that seeking support is not a sign of weakness; it’s an empowering step toward reclaiming your sense of self and reality amidst the challenges posed by DPDR.
Depersonalization and derealization disorder, as outlined in the DSM-5, is a dissociative disorder characterized by persistent or recurrent feelings of detachment from one’s self (depersonalization) or surroundings (derealization). These experiences can be distressing and interfere with daily functioning. For a deeper understanding of this disorder, you can explore an insightful article on the topic by visiting Unplugged Psych.
LEARN MORE About Unmasking the Mysteries Behind Depersonalization and Derealization
FAQs
What is depersonalization and derealization disorder?
Depersonalization and derealization disorder is a mental health condition characterized by a persistent or recurrent feeling of being detached from one’s body (depersonalization) or feeling that the world around them is unreal or distorted (derealization).
What are the symptoms of depersonalization and derealization disorder?
Symptoms of depersonalization and derealization disorder may include feeling like an outside observer of one’s thoughts, feelings, and actions (depersonalization), feeling like the world is unreal or distorted (derealization), emotional numbness, and a sense of detachment from oneself or one’s surroundings.
What are the causes of depersonalization and derealization disorder?
The exact cause of depersonalization and derealization disorder is not fully understood, but it is believed to be related to a combination of biological, psychological, and environmental factors. Trauma, stress, anxiety, and certain personality traits may contribute to the development of the disorder.
How is depersonalization and derealization disorder diagnosed?
Depersonalization and derealization disorder is diagnosed based on a thorough psychiatric evaluation, including a discussion of symptoms, medical history, and ruling out other potential causes. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) provides criteria for diagnosing the disorder.
What are the treatment options for depersonalization and derealization disorder?
Treatment for depersonalization and derealization disorder may include psychotherapy, medication, and stress-reduction techniques. Cognitive-behavioral therapy (CBT) and mindfulness-based approaches have shown some effectiveness in helping individuals manage symptoms.
Is depersonalization and derealization disorder a common condition?
Depersonalization and derealization disorder is considered relatively rare, with prevalence estimates ranging from 1-2% of the general population. However, it is possible that the disorder is underreported due to stigma and lack of awareness.




