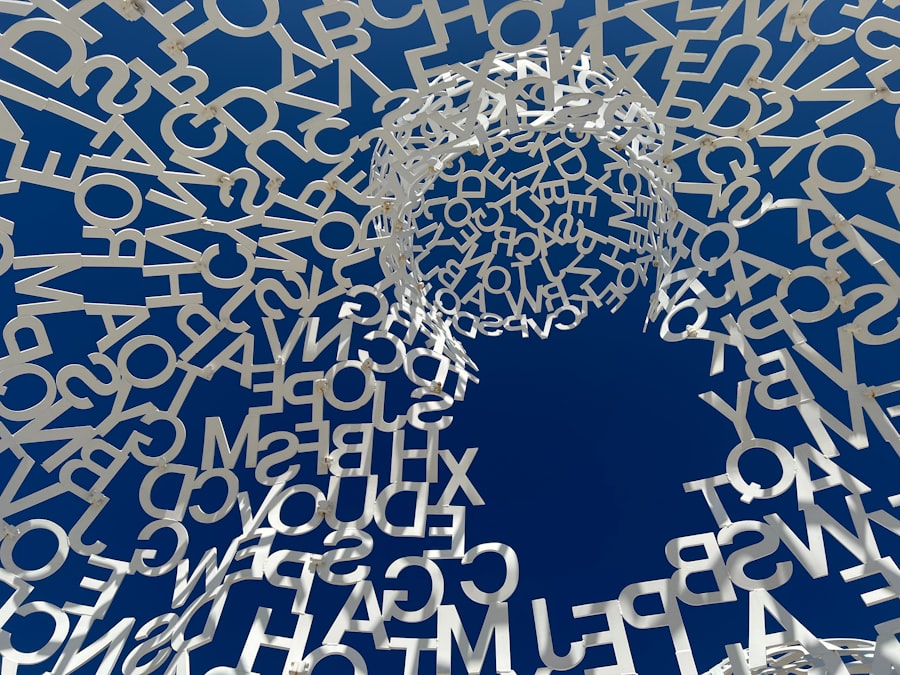
You are embarking on a journey to understand a phenomenon you might have experienced or heard about: depersonalization. This state, often described as feeling detached from yourself, your thoughts, feelings, or body, can be disorienting and unsettling. It’s like watching your own life unfold from a distance, as if you’re an actor in a play, observing your character without inhabiting it. This article will guide you through the intricacies of depersonalization, outlining its nature, causes, symptoms, and potential avenues for coping and recovery.
Depersonalization is a dissociative symptom and can also be a core feature of a dissociative disorder. To truly grasp it, you must first understand the fundamental concept of dissociation.
Dissociation as a Spectrum
Imagine dissociation as a spectrum, much like light. At one end, you have everyday experiences of mild dissociation: daydreaming during a boring meeting, getting lost in a book, or driving a familiar route and realizing you don’t recall the last few miles. These are common and generally harmless. On the other end of the spectrum lies severe dissociative disorders, where disruptions in memory, identity, emotion, perception, and consciousness are profound and debilitating. Depersonalization resides on this spectrum, often occupying a space where the disruption is noticeable and distressing but not necessarily as pervasive as in some other dissociative conditions. You may find yourself oscillating between moments of feeling fully present and moments of profound detachment.
Defining Depersonalization
Depersonalization, specifically, is characterized by persistent or recurrent experiences of feeling detached from your own mental processes or body, as if you are an outside observer of your life. It’s as if a veil has been drawn between you and your internal experience. You might describe it as feeling unreal, foggy, or robotic. This isn’t psychosis; you understand that this feeling is not normal and that your sense of detachment is an internal experience, not an external reality. You retain your grasp on reality, differentiating it from hallucinations or delusions. This critical distinction sets depersonalization apart from psychotic disorders.
Relationship to Derealization
It’s crucial to understand that depersonalization often co-occurs with derealization. While depersonalization involves detachment from yourself, derealization is the feeling of detachment from your surroundings. The world around you may seem unreal, dreamlike, foggy, or distorted. Objects might appear flat, colorless, or farther away than they are. People might feel unfamiliar, robotic, or like characters in a play. Think of it as a double whammy: you’re feeling unreal, and the world around you feels equally unreal. This dual experience is often referred to as Depersonalization-Derealization Disorder (DPDR). You may find one experience more prominent than the other, but they are often intertwined.
Depersonalization is a fascinating yet complex psychological phenomenon that can significantly impact an individual’s sense of self and reality. For those interested in exploring this topic further, a related article can be found on Unplugged Psychology, which delves into the intricacies of depersonalization and its effects on mental health. You can read more about it by visiting this link: Unplugged Psychology.
The Causes and Triggers of Depersonalization
Understanding why you might experience depersonalization requires looking at a complex interplay of environmental, psychological, and biological factors. It’s rarely a single cause but rather a convergence of vulnerabilities and stressors.
Trauma and Stress
This is perhaps the most significant and well-documented trigger. You will often find that depersonalization is a protective mechanism your psyche employs to cope with overwhelming experiences. When faced with severe trauma, particularly prolonged or repeated trauma (such as childhood abuse, neglect, or chronic emotional invalidation), your brain might instinctively create a psychological distance from the pain. It’s like your mind is hitting a “disconnect” button to protect itself from unbearable emotional agony. You might experience this as a response to:
- Acute Traumatic Events: A life-threatening accident, a violent assault, or witnessing a horrific event can induce a temporary or prolonged state of depersonalization.
- Chronic Stress: Persistent high-stress environments, such as a demanding job, an unhealthy relationship, or financial difficulties, can gradually erode your sense of presence and ground you in the present moment. Your nervous system becomes overtaxed, leading to a feeling of burnout and detachment.
- Childhood Adversity: Early experiences of abuse, neglect, or unpredictable environments can significantly increase your vulnerability to dissociative symptoms later in life. Your brain learns to dissociate as a coping mechanism from an early age, a pattern that can become deeply ingrained.
Anxiety and Panic Disorders
A profound link exists between depersonalization and anxiety, particularly panic disorder. When you experience a panic attack, the surge of adrenaline and physiological arousal can be incredibly frightening. Your body’s fight-or-flight response goes into overdrive, and in some individuals, this intense physiological discomfort can trigger a feeling of unreality or detachment. You might feel like you’re going crazy, dying, or losing control, and depersonalization becomes a terrifying accompaniment to these sensations. The fear of depersonalization itself can then perpetuate a cycle of anxiety, making you hypervigilant to any sensory shift that might indicate another episode. You become trapped in a feedback loop.
Substance Use
Certain substances can induce or exacerbate depersonalization.
- Cannabis: While often perceived as relaxing, cannabis can paradoxically trigger anxiety and depersonalization in some individuals, especially with high doses or in those with pre-existing vulnerabilities. You might find yourself feeling profoundly detached and paranoid after using it.
- Psychedelics: Substances like LSD, psilocybin, and MDMA can induce profound alterations in perception and consciousness. While some people report positive experiences, others can experience intense depersonalization, derealization, or even persistent perceptual distortions long after the drug’s effects have worn off.
- Stimulants: High doses of stimulants can lead to anxiety, paranoia, and a sense of unreality, potentially contributing to depersonalization episodes.
Other Factors
Beyond these primary triggers, a multitude of other factors can contribute to or exacerbate depersonalization:
- Lack of Sleep: Chronic sleep deprivation can significantly impact your cognitive function and emotional regulation, making you more susceptible to feelings of fog and unreality.
- Depression: While distinct, depersonalization can be a symptom of severe depression, particularly if you experience profound anhedonia (inability to feel pleasure) or emotional numbness.
- Medication Side Effects: Certain medications, particularly some anxiolytics or antidepressants, can have side effects that include feelings of detachment or unreality.
- Neurological Conditions: Though less common, certain neurological conditions or brain injuries can, in rare instances, be associated with dissociative symptoms.
The Symptoms and Experiential Qualities
To recognize depersonalization in yourself or others, you need a detailed understanding of its varied manifestations. You may not experience all of these, but a significant portion will likely resonate if you are experiencing depersonalization.
Altered Sense of Self
This is the core of depersonalization. You often describe this in vivid and sometimes unsettling metaphors.
- Observing Yourself from Outside: You might feel like you are watching yourself as if from a few feet away, or even from above your body. It’s like being a spectator to your own life, rather than an active participant. Your actions feel pre-programmed or automated.
- Feeling Robotic or Automatic: You perform daily tasks, but it feels like you’re going through the motions without genuine engagement. Your movements might feel unnatural or disconnected from your will. You are a puppet, and someone else is pulling the strings.
- Emotional Numbness: This is a particularly distressing symptom. You might find yourself unable to feel emotions, even in situations where you “should” feel joy, sadness, fear, or anger. It’s not that the emotions aren’t there, but rather that you can’t access them, like a radio playing static instead of music. This can lead to significant distress and difficulty in relationships.
- Loss of Sense of Identity: You may question who you are, or feel like your personality has changed. Your past memories might feel like someone else’s story, lacking emotional resonance. Your reflection in a mirror might seem unfamiliar or even startling.
- Changes in Body Perception: Your limbs might feel distant, heavy, light, or alien. Your hands might not feel like your own, or you might perceive parts of your body as distorted in size or shape. This is not a hallucination, but a subjective alteration of how you perceive your physical form.
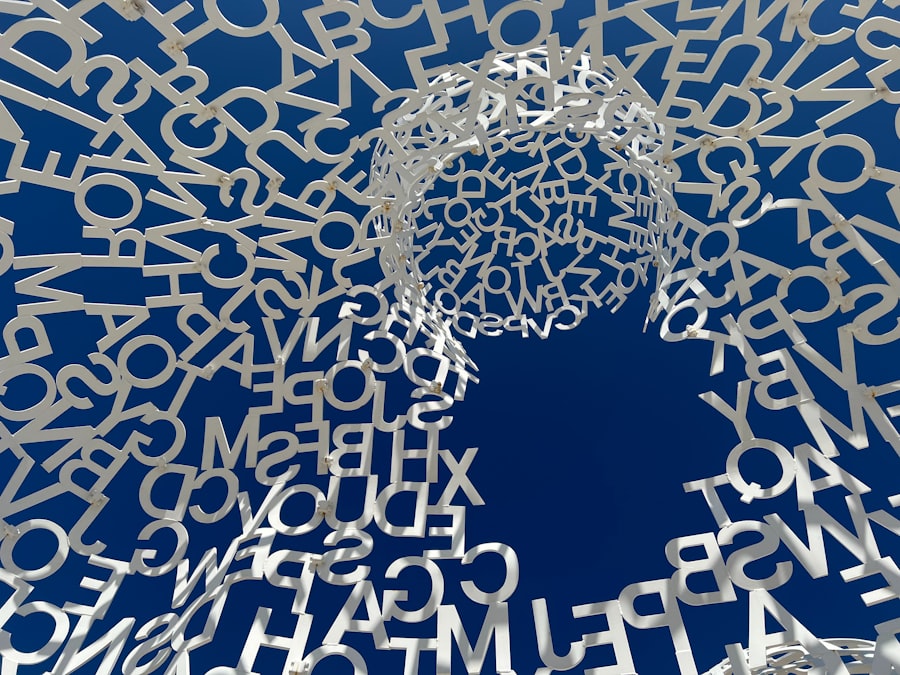
Cognitive and Perceptual Distortions
Beyond the self, depersonalization often brings with it a host of cognitive and perceptual abnormalities.
- Foggy or Hazy Thinking: Your thoughts might feel unclear, slowed down, or difficult to grasp. It’s like navigating a dense mental fog, making concentration and decision-making challenging.
- Memory Impairment: While not amnesia, you might find it hard to recall specific details of recent events, or your memories might lack the usual emotional or personal connection. They feel abstract, like facts you’ve learned from a book, rather than lived experiences.
- Altered Time Perception: Time might feel like it’s speeding up or slowing down drastically. Minutes can stretch into hours, or entire days can pass in a blur. This contributes to the feeling of unreality.
- Sensory Blunting or Over-stimulation: Paradoxically, you might experience either a dulling of your senses (foods taste bland, familiar sounds seem distant) or an uncomfortable hypersensitivity (noises are too loud, lights are too bright), contributing to the feeling of being overwhelmed and disconnected.
Impact on Daily Functioning
The pervasive nature of depersonalization can significantly disrupt your daily life.
- Social Isolation: The difficulty in feeling emotions and connecting with others can lead you to withdraw from social interactions. You might feel like you’re faking empathy or just observing conversations, making genuine connection difficult.
- Occupational or Academic Difficulties: Concentration issues, memory problems, and a general lack of motivation can impair your performance at work or school. You might struggle to complete tasks or engage with your responsibilities.
- Relationship Strain: Your loved ones may find it challenging to understand what you’re going through, and your emotional distance can create rifts in your relationships. It’s hard to be close to someone who feels like an empty vessel.
- Fear and Anxiety: The experience of depersonalization itself is often terrifying. The fear of losing your mind, of becoming permanently disconnected, or of the sensations never ending, can be a source of significant anxiety and lead to a vicious cycle.
Diagnosis and Differential Diagnosis
Diagnosing depersonalization requires careful evaluation, as its symptoms can overlap with other conditions. You will likely undergo a thorough assessment by a mental health professional.
Diagnostic Criteria (DSM-5)
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), Depersonalization-Derealization Disorder is diagnosed when you meet specific criteria:
- Persistent or Recurrent Experiences of Depersonalization, Derealization, or Both: You must experience these symptoms repeatedly or continuously.
- Reality Testing Remains Intact: Crucially, you understand that these experiences are not real, or are subjective alterations, and you do not lose touch with reality (e.g., you know your body is real, even if it doesn’t feel like it). This distinguishes it from psychotic disorders.
- Significant Distress or Impairment: The symptoms must cause you significant distress or impairment in social, occupational, or other important areas of functioning.
- Symptoms Not Attributable to a Substance or Other Medical Condition: The symptoms cannot be better explained by the physiological effects of a substance (e.g., illicit drugs, medication) or another medical condition (e.g., epilepsy, head trauma).
- Symptoms Not Better Explained by Another Mental Disorder: Your symptoms are not better accounted for by another mental disorder, such as panic disorder, major depressive disorder, psychotic disorders, or another dissociative disorder (e.g., dissociative identity disorder).
Ruling Out Other Conditions
A crucial part of the diagnostic process involves ruling out other conditions that might mimic depersonalization. This is where your mental health professional acts as a detective.
- Anxiety Disorders: While depersonalization can be a symptom of panic attacks, chronic depersonalization as a standalone disorder needs to be distinguished from primary anxiety.
- Depressive Disorders: Profound emotional numbness can occur in severe depression, but depersonalization disorder is characterized by a specific feeling of detachment from self or surroundings, rather than just general anhedonia.
- Psychotic Disorders (e.g., Schizophrenia): The key differentiator here is intact reality testing in depersonalization. Individuals with psychosis genuinely believe their altered perceptions are real. You, with depersonalization, know something is “off.”
- Neurological Conditions: Conditions like temporal lobe epilepsy or migraines can sometimes cause transient feelings of unreality. A medical workup may be necessary to rule these out.
- Substance-Induced Disorders: It’s vital to assess your substance use history, as many substances can directly induce depersonalization.
Depersonalization is a fascinating area within psychology that explores the feeling of being detached from oneself or one’s surroundings. For those interested in delving deeper into this topic, a related article can be found at Unplugged Psych, which discusses various aspects of depersonalization and its impact on mental health. This resource provides valuable insights and can help readers better understand the complexities of this phenomenon.
Coping Mechanisms and Treatment Approaches
| Metric | Description | Typical Range/Value | Measurement Method |
|---|---|---|---|
| Depersonalization Severity Score | Quantifies the intensity of depersonalization symptoms | 0-100 (higher scores indicate greater severity) | Cambridge Depersonalization Scale (CDS) |
| Frequency of Episodes | Number of depersonalization episodes experienced per week | 0 to multiple times daily | Self-report diary or clinical interview |
| Duration of Episodes | Average length of each depersonalization episode | Seconds to hours | Self-report or clinical observation |
| Associated Anxiety Level | Degree of anxiety accompanying depersonalization | Measured on a scale of 0-10 | Beck Anxiety Inventory (BAI) or similar scales |
| Functional Impairment | Impact of depersonalization on daily functioning | None, mild, moderate, severe | Clinical assessment or WHO Disability Assessment Schedule |
| Onset Age | Typical age when depersonalization symptoms first appear | Late adolescence to early adulthood (15-25 years) | Clinical history |
| Comorbidity Rate | Percentage of individuals with depersonalization also diagnosed with anxiety or depression | Up to 80% | Clinical diagnosis and structured interviews |
If you are experiencing depersonalization, know that there are strategies and treatments that can help you regain a sense of groundedness and connection. It’s a journey, not a switch, but recovery is possible.
Therapeutic Interventions
Psychotherapy is often the cornerstone of treatment for depersonalization-derealization disorder.
- Cognitive Behavioral Therapy (CBT): CBT is highly effective in helping you understand and manage the thoughts and behaviors associated with depersonalization. It works by:
- Identifying Triggers: Helping you recognize the situations, thoughts, or feelings that precipitate depersonalization episodes.
- Cognitive Restructuring: Challenging and changing maladaptive thought patterns that perpetuate the detachment (e.g., “I’m going crazy,” “This will never end”). You learn to reframe catastrophic thoughts.
- Behavioral Activation: Encouraging engagement in activities that bring you pleasure or a sense of accomplishment, even if you don’t “feel” like it, to counteract withdrawal and foster a sense of presence.
- Exposure Therapy: Gradually exposing you to situations or sensations that trigger depersonalization in a controlled way, helping you learn that these feelings are temporary and harmless.
- Dialectical Behavior Therapy (DBT): Originally developed for borderline personality disorder, DBT’s emphasis on mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness can be highly beneficial. The mindfulness component, in particular, can help you anchor yourself in the present moment.
- Psychodynamic Therapy or Trauma-Informed Therapy: If your depersonalization is rooted in past trauma, exploring and processing these experiences in a safe therapeutic environment can be vital. These therapies help you understand the unconscious dynamics and past events that contributed to your dissociative coping mechanisms.
- Grounding Techniques: These are practical strategies you can use in the moment to counteract feelings of unreality and bring your attention back to your body and surroundings. Examples include:
- 5-4-3-2-1 Technique: Naming 5 things you can see, 4 things you can feel, 3 things you can hear, 2 things you can smell, and 1 thing you can taste.
- Physical Sensations: Holding ice cubes, splashing cold water on your face, feeling the texture of an object, pressing your feet firmly into the ground.
- Intense Flavors/Smells: Sucking on a sour candy, chewing strong gum, smelling something pungent like essential oils.
Pharmacological Approaches
While there isn’t a specific medication for depersonalization itself, medications can be helpful in treating co-occurring conditions that exacerbate it.
- Antidepressants (SSRIs): Selective serotonin reuptake inhibitors (SSRIs) are often prescribed to address underlying anxiety, panic disorder, or depression, which frequently co-occur with and can worsen depersonalization. By reducing anxiety, the frequency and intensity of depersonalization episodes can decrease.
- Anxiolytics: In some cases, short-term use of benzodiazepines might be considered for acute, severe anxiety or panic attacks, but their long-term use is generally discouraged due to potential for dependence.
- Other Medications: Your doctor may explore other options depending on your specific symptoms and medical history. However, you should approach medication with a balanced perspective, as it’s often a supportive measure rather than a cure for depersonalization itself.
Self-Help and Lifestyle Adjustments
Beyond professional help, you can adopt several self-help strategies and make lifestyle changes to support your recovery.
- Education and Understanding: Simply understanding what depersonalization is can be immensely empowering. Knowing that you are not alone and that it’s a recognized, treatable condition can reduce your fear and anxiety.
- Mindfulness and Meditation: Regular practice of mindfulness can help you cultivate present-moment awareness and observe your thoughts and feelings without judgment, fostering a stronger connection to your internal experience.
- Regular Exercise: Physical activity can reduce stress, improve mood, and help you feel more embodied and connected to your physical self.
- Adequate Sleep: Prioritize good sleep hygiene. A well-rested brain is better equipped to manage stress and maintain a sense of reality.
- Balanced Diet: Nutritional deficiencies or irregular eating patterns can impact your mood and energy levels, potentially exacerbating symptoms.
- Stress Management Techniques: Identify and implement healthy ways to manage stress, such as yoga, deep breathing exercises, spending time in nature, or engaging in hobbies.
- Limiting Stimulants and Substances: Reducing or eliminating caffeine, nicotine, alcohol, and illicit drugs can significantly improve symptoms, especially as these substances can trigger or worsen depersonalization.
- Support Groups: Connecting with others who share similar experiences can provide validation, reduce feelings of isolation, and offer practical coping strategies.
Understanding depersonalization is a crucial step towards managing and ultimately overcoming it. By recognizing its nature, identifying potential causes, understanding its symptoms, and actively engaging in therapeutic and self-help strategies, you can begin to peel back the layers of detachment and return to a more grounded, lived experience of yourself and the world around you. You are on a path towards reclaiming your sense of presence.
FAQs
What is depersonalization in psychology?
Depersonalization is a psychological condition characterized by a feeling of detachment or estrangement from one’s own body, thoughts, or emotions. Individuals may feel as though they are observing themselves from outside their body or that their surroundings are unreal.
What causes depersonalization?
Depersonalization can be triggered by severe stress, trauma, anxiety, or substance use. It is often associated with other mental health conditions such as depression, panic disorder, or post-traumatic stress disorder (PTSD).
How is depersonalization diagnosed?
Diagnosis typically involves a clinical interview where a mental health professional assesses symptoms and rules out other medical or psychiatric conditions. The diagnosis may be part of depersonalization-derealization disorder if symptoms are persistent and cause significant distress.
What treatments are available for depersonalization?
Treatment options include psychotherapy, particularly cognitive-behavioral therapy (CBT), which helps individuals manage symptoms and underlying issues. In some cases, medication may be prescribed to address co-occurring conditions like anxiety or depression.
Is depersonalization a permanent condition?
Depersonalization is often temporary and can improve with treatment and time. However, for some individuals, it may become chronic. Early intervention and support can improve outcomes and help manage symptoms effectively.