You’ve likely experienced it: that fleeting, unsettling sensation where a new moment feels inexplicably familiar, as if you’ve lived it before. This is déjà vu, a French term meaning “already seen.” While commonly dismissed as a trivial quirk of the mind, neurologists delve deeper, viewing it as a window into the intricate workings of your brain. Instead of a supernatural omen, you should understand déjà vu as a brief, benign neurological glitch, a whisper from your cognitive machinery.
To comprehend frequent déjà vu, you must first grasp its neurological foundations. Your brain is a complex symphony of electrochemical signals, constantly processing, storing, and retrieving information. Déjà vu, in essence, represents a momentary discord in this symphony. It’s not a memory being retrieved, but rather the feeling of memory retrieval, without an actual preceding event.
The Temporal Lobe: A Key Player
The temporal lobe, located on the side of your brain, plays a critical role in memory formation (particularly declarative memory, which includes facts and events), language comprehension, and emotional processing. Scientists have long linked activity in this region to déjà vu.
- Hippocampus Involvement: Within the temporal lobe lies the hippocampus, a seahorse-shaped structure vital for converting short-term memories into long-term ones. Researchers hypothesize that a momentary misfiring or overactivation of the hippocampus can trick your consciousness into perceiving a new experience as an old one. Imagine your brain as a filing cabinet; the hippocampus is the diligent archivist. During déjà vu, it mistakenly tags a new file as an existing one, creating the illusion of prior acquaintance.
- Rhinal Cortex Connection: Adjacent to the hippocampus are the rhinal cortices, which are also involved in memory. Some theories suggest that a mismatch between the input from the perirhinal cortex (involved in recognizing objects and familiar landscapes) and the parahippocampal cortex (involved in spatial memory) could contribute to the déjà vu phenomenon. Your brain is trying to match a face to a name, but the two come from slightly different, misaligned directories.
Disruption in Memory Processing
At its core, déjà vu is often considered a disruption in your brain’s memory processing system. It’s not a failure to encode a memory, but rather an unusual way in which your brain accesses or interprets that encoding.
- Dual Processing Theory: One prominent theory suggests that your brain has two parallel memory processing streams. During déjà vu, one stream might process an incoming sensory experience slightly before the other. When the second stream catches up, it perceives the delayed input from the first stream as an “already processed” event, leading to the sensation of familiarity. Think of it like two internal clocks, momentarily out of sync.
- Attentional Lags: Another hypothesis posits that déjà vu can arise when your attention is split or fleeting. You might initially perceive a scene or event without fully registering it. When your attention then fully focuses on it, your brain interprets this as a second, familiar exposure, even though it’s the first conscious recognition. It’s like glancing at a word without reading it, then rereading it and feeling a vague sense of familiarity.
If you’re interested in understanding the neurological aspects of frequent déjà vu experiences, you might find the article on Unplugged Psych particularly enlightening. It delves into the potential causes and implications of this phenomenon from a neurologist’s perspective. For more information, you can read the article here: Unplugged Psych.
When Frequent Déjà Vu Becomes a Concern
While occasional déjà vu is a universal experience, occurring in an estimated 60-80% of you, frequent or persistent déjà vu warrants closer examination. It’s like a distant train whistle; a rare occurrence is normal, but constant whistling might signal an issue with the tracks.
Temporal Lobe Epilepsy
The most significant neurological connection to frequent déjà vu is temporal lobe epilepsy (TLE). For individuals with TLE, déjà vu can be an “aura” or a warning sign preceding a seizure.
- Focal Seizures: In TLE, seizures often originate in the temporal lobe. These are typically focal seizures, meaning they affect only one part of the brain. The déjà vu experience during TLE can be more intense, prolonged, and accompanied by other symptoms such as unusual smells or tastes, a rising sensation in the stomach, or a feeling of detachment.
- Distinguishing Benign Déjà Vu from Epileptic Aura: If you experience déjà vu with increasing frequency, or if it’s accompanied by other unusual sensations, strange smells, or a sense of fear or unreality, you should consult a neurologist. The benign type is fleeting and rarely unsettling; the epileptic type can be a precursor to a more significant event.
Other Neurological Conditions
While less common than TLE, other neurological conditions can also contribute to more frequent déjà vu.
- Migraine with Aura: Some individuals who experience migraines with aura (sensory disturbances preceding the headache) report a heightened incidence of déjà vu alongside their other aura symptoms. This suggests a shared neurological pathway or a general propensity for altered sensory processing.
- Dementia and Memory Impairment: In some cases of early-stage dementia, particularly those affecting the temporal lobes, increased déjà vu can be observed. This is likely due to the progressive disruption of memory pathways, leading to more frequent misfirings or misinterpretations of sensory input. Your brain’s filing system is becoming disarrayed, leading to more “misfiled” experiences.
The Psychological Dimensions of Déjà Vu
Beyond the purely neurological, there are psychological factors that can influence the frequency and intensity of your déjà vu experiences. Your mental state is not merely a passenger in your brain; it actively shapes its landscape.
Stress and Fatigue
Just as stress and fatigue can make you more prone to forgetfulness or errors in judgment, they can also contribute to an increase in déjà vu.
- Cognitive Load: When your brain is under immense cognitive load from stress or lacks adequate rest, its normal processing efficiency can decline. This makes it more susceptible to inconsistencies in memory retrieval and perception, potentially leading to more frequent déjà vu. Imagine your computer running too many programs at once; errors are more likely.
- Attentional Deficits: Stress often leads to fragmented attention. As discussed earlier, a fragmented initial perception of an event, followed by a more focused re-evaluation, can trigger déjà vu. You’re simply not “present” enough in the first instance.
Personality and Trait Factors
Research suggests that certain personality traits might correlate with a higher incidence of déjà vu.
- Openness to Experience: Individuals who score highly on “openness to experience” (a Big Five personality trait characterized by curiosity, imagination, and a preference for novelty) tend to report experiencing déjà vu more often. This could be due to a greater internal awareness or a tendency to notice nuanced subjective experiences.
- Anxiety and Depression: While not a causal link, a correlation has been observed between individuals experiencing high levels of anxiety or depression and an increased report of déjà vu. This might be due to heightened self-monitoring or an increased focus on internal states, making such experiences more salient.
Diagnostic Approaches for Frequent Déjà Vu

If you are experiencing frequent déjà vu, especially if it’s accompanied by other concerning symptoms, a neurologist will typically undertake a systematic diagnostic process. This isn’t about proving you have déjà vu, but rather ruling out neurological conditions that could be causing it.
Neurological Examination
The initial step will involve a comprehensive neurological examination. This helps your doctor assess your overall neurological health.
- Assessment of Reflexes, Coordination, and Sensation: Your neurologist will check your reflexes, muscle strength, coordination, balance, and sensory perception. Abnormalities in these areas could indicate underlying neurological issues beyond just déjà vu.
- Cognitive Function Tests: Simple cognitive tests might be administered to assess your memory, attention, language skills, and other cognitive domains. These help identify any subtle cognitive deficits that could be related to your symptoms.
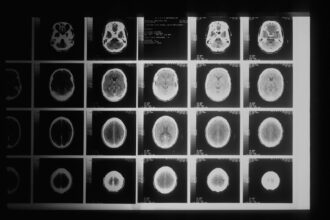
Advanced Imaging Techniques
To visualize the structure and function of your brain, your neurologist may order advanced imaging studies.
- Magnetic Resonance Imaging (MRI): An MRI scan provides detailed images of your brain’s structure. It can detect structural abnormalities such as tumors, lesions, or atrophy (shrinkage) in areas like the temporal lobe that might contribute to seizures or cognitive impairment. Think of it as a detailed blueprint of your brain’s architecture.
- Functional MRI (fMRI): While less commonly used specifically for déjà vu diagnosis, fMRI can measure brain activity by detecting changes in blood flow. It could potentially show abnormal activity patterns in specific brain regions during or between episodes.
Electroencephalogram (EEG)
An EEG is a crucial tool for diagnosing conditions like epilepsy.
- Recording Brain Electrical Activity: An EEG involves placing electrodes on your scalp to record the electrical activity of your brain. It can detect abnormal brain wave patterns that are characteristic of seizure activity, even subclinical (without outward symptoms) seizures. It’s like listening to the electrical hum of your brain to detect any unusual rhythms.
- Long-Term Monitoring: In some cases, if routine EEG doesn’t capture abnormal activity, your neurologist might recommend long-term EEG monitoring (either in-hospital or ambulatory) to increase the chances of recording an event.
Frequent episodes of déjà vu can be a perplexing experience, often prompting individuals to seek insights from specialists such as neurologists. Understanding the underlying mechanisms of this phenomenon can shed light on its connection to memory and perception. For those interested in exploring this topic further, a related article discusses various aspects of déjà vu and its implications on mental health. You can read more about it in this informative piece here.
Management and Outlook
| Metric | Details |
|---|---|
| Common Causes | Temporal lobe epilepsy, migraines, anxiety disorders, brain lesions |
| Typical Patient Age | 20-40 years |
| Frequency of Déjà Vu Episodes | Varies from occasional to multiple times daily |
| Diagnostic Tests | EEG, MRI, neurological examination, neuropsychological testing |
| Treatment Options | Medication (antiepileptics), cognitive therapy, stress management |
| Referral to Neurologist Recommended When | Déjà vu episodes are frequent, prolonged, or associated with other neurological symptoms |
| Prevalence of Frequent Déjà Vu | Rare, exact prevalence unknown |
For most people, frequent déjà vu is a benign phenomenon that requires no specific treatment. However, if it’s linked to an underlying condition, managing that condition is key.
Addressing Underlying Conditions
If your frequent déjà vu is diagnosed as a symptom of temporal lobe epilepsy, treatment will focus on managing the seizures.
- Antiepileptic Medications (AEDs): These are the cornerstone of epilepsy treatment. Various AEDs are available, and your neurologist will work with you to find the most effective medication and dosage to control your seizures and reduce the frequency of your déjà vu auras.
- Lifestyle Modifications: Alongside medication, lifestyle adjustments such as ensuring adequate sleep, managing stress, and avoiding seizure triggers can significantly help.
Coping Strategies for Benign Déjà Vu
If your neurologist determines your frequent déjà vu is benign, you have strategies to cope with the experience.
- Reassurance and Education: Simply understanding the neurological basis of déjà vu can reduce anxiety about the experience. Knowing it’s a normal brain glitch, not a sign of impending doom, can bring significant relief.
- Mindfulness and Grounding Techniques: When déjà vu strikes, practicing mindfulness can help. Focus on your immediate surroundings, engage your senses, and remind yourself that the moment is new. Grounding techniques, like naming five things you can see, four you can touch, three you can hear, two you can smell, and one you can taste, can help reorient you to the present. You’re consciously pulling your attention back to the current reality, countering your brain’s momentary delusion.
In conclusion, you should view déjà vu, in its frequent manifestation, not as an anomaly of fate, but as a fascinating signal from your brain. While typically harmless, its increased recurrence serves as a call to attention, urging you to explore the subtle, yet profound, mechanisms governing your perception and memory. By understanding these neurological insights, you gain a deeper appreciation for the intricate and often enigmatic power of your own mind.
FAQs
What is déjà vu and why does it occur frequently in some people?
Déjà vu is the sensation that a current experience has been lived through before. It occurs due to a temporary glitch in the brain’s memory processing, often involving the temporal lobe. Frequent déjà vu can be linked to neurological conditions or stress, and may warrant medical evaluation.
When should someone see a neurologist for frequent déjà vu?
If déjà vu episodes happen very often, last longer than usual, or are accompanied by other symptoms like confusion, memory loss, or seizures, it is advisable to consult a neurologist. Frequent déjà vu can sometimes be a sign of temporal lobe epilepsy or other neurological disorders.
What tests might a neurologist perform to diagnose the cause of frequent déjà vu?
A neurologist may conduct a detailed medical history and neurological examination, followed by diagnostic tests such as an EEG (electroencephalogram) to detect abnormal brain activity, MRI scans to look for structural brain abnormalities, and possibly neuropsychological assessments.
Can frequent déjà vu be treated or managed?
Treatment depends on the underlying cause. If frequent déjà vu is related to epilepsy, anti-seizure medications may be prescribed. For other causes, managing stress, improving sleep, and addressing any neurological conditions can help reduce episodes. A neurologist can recommend appropriate treatment plans.
Is frequent déjà vu dangerous or a sign of a serious condition?
While occasional déjà vu is common and harmless, frequent or intense episodes can sometimes indicate neurological issues such as epilepsy. It is important to seek medical advice to rule out serious conditions and receive proper care if needed.