The dorsal vagal shutdown response is a physiological and psychological state of immobility and dissociation, originating from the most ancient branch of the vagus nerve – the dorsal vagal complex (DVC). This response is a primal survival mechanism, active when the organism perceives an overwhelm or life threat from which fight or flight is not possible. Imagine a prey animal playing dead; this is a vivid representation of a dorsal vagal shutdown. It is not a conscious choice but an automatic, involuntary collapse of the nervous system, intended to conserve energy, minimize pain, and avoid further trauma. When you experience this, your body essentially goes “offline” to cope with an unmanageable situation.
The Neurobiology of Shutdown
To comprehend the dorsal vagal shutdown, you must first understand the Polyvagal Theory, developed by Stephen Porges. This theory posits that the autonomic nervous system is not a simple dichotomy of sympathetic and parasympathetic, but rather a more complex hierarchical system. The vagus nerve, a cranial nerve that meanders through the body, plays a central role. It has two main branches: the ventral vagal complex (VVC) and the dorsal vagal complex (DVC).
- Ventral Vagal Complex (VVC): This is the more recently evolved branch, associated with social engagement, connection, and feelings of safety. When you are in a state of ventral vagal activation, you feel calm, connected, and capable of empathy. It allows for flexible and nuanced responses to your environment.
- Dorsal Vagal Complex (DVC): This is the oldest branch, responsible for basic bodily maintenance like digestion and heart rate, but also for immobilisation responses. It’s what drives the “freeze” response, and in extreme cases, the “shutdown” response.
When your nervous system detects overwhelming threat, and fight or flight responses are deemed ineffective or unsafe, it defaults to the DVC. This is a brilliant survival mechanism in situations of genuine, inescapable danger, akin to a circuit breaker preventing a complete system meltdown. However, in modern life, this response can be triggered by perceived threats that are not life-threatening, such as chronic stress, emotional neglect, or overwhelming social situations. Your body reacts as if it’s in mortal peril, even when the threat is purely psychological or social.
Recognizing the Signs of Shutdown
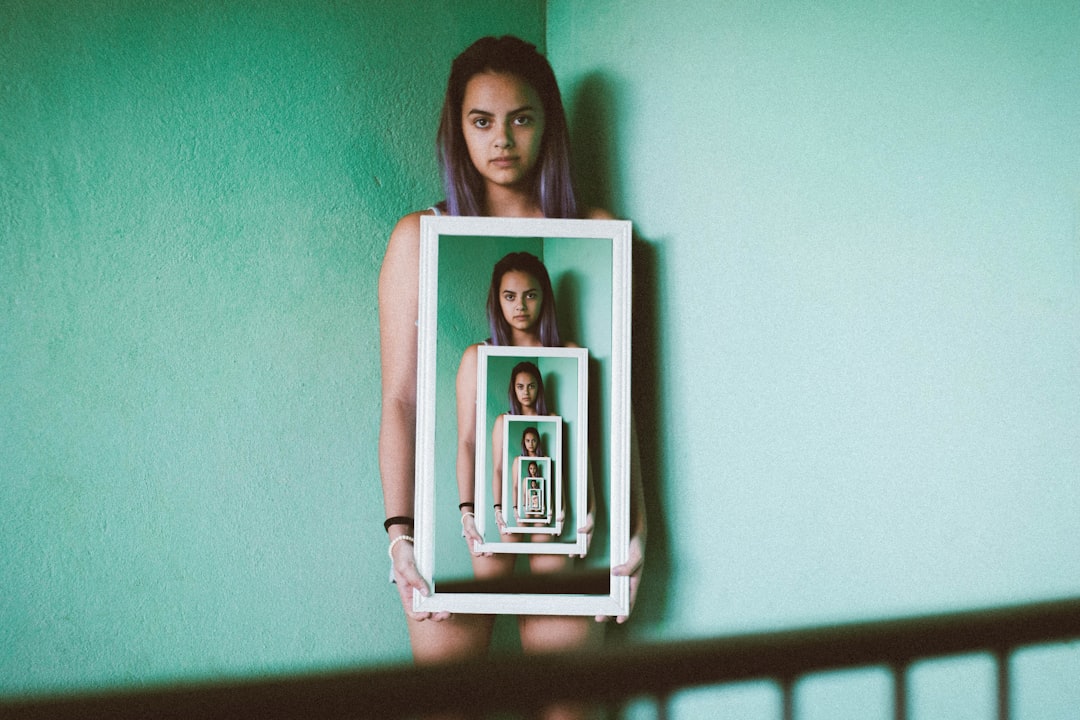
Identifying a dorsal vagal shutdown in yourself is the crucial first step toward healing. Because this state is characterized by a profound disconnection, self-awareness can be significantly impaired. It’s not simply feeling tired or sad; it’s a deep physiological and psychological deactivation.
- Physical Manifestations: You might experience a noticeable drop in energy, extreme fatigue, and a feeling of bodily heaviness. Your heart rate may slow significantly, your breathing might become shallow, and your limbs might feel numb or heavy. Digestion can slow or halt entirely, leading to nausea or constipation. Your muscles might feel slack or limp, rather than tense.
- Emotional and Cognitive Symptoms: A defining characteristic is a sense of emotional numbness or detachment. You may feel flat, empty, or anhedonic (unable to experience pleasure). Dissociation is common, causing a feeling of unreality, as if you are observing your life from outside your body. There might be a sense of hopelessness, helplessness, and a profound resignation. Cognitive function can be impaired, leading to difficulty concentrating, memory issues, and a sense of mental fog.
- Behavioral Indicators: You might withdraw socially, become inactive, and struggle to initiate or complete tasks. There can be a desire to hide or disappear, and a profound lack of motivation. When in this state, simple activities can feel overwhelmingly effortful, leading to procrastination or paralysis.
It is important to differentiate shutdown from depression or anxiety, although there can be significant overlap. While depression often involves sadness and a lack of energy, dorsal vagal shutdown is more about a complete physiological and psychological “turning off.” Anxiety, conversely, is typically characterized by heightened sympathetic nervous system arousal (fight or flight). Understanding this distinction helps you tailor your healing approach more effectively.
Healing the dorsal vagal shutdown response is a crucial aspect of trauma recovery and emotional regulation. For those interested in exploring this topic further, a related article can be found on Unplugged Psych, which delves into various techniques and therapies aimed at reactivating the nervous system and promoting healing. You can read more about it by visiting this link: Unplugged Psych. This resource provides valuable insights and practical strategies for individuals seeking to overcome the effects of trauma and enhance their overall well-being.
The Triggers of Dorsal Vagal Shutdown
Understanding what moves you into a shutdown state is paramount for self-regulation and prevention. Triggers are highly individual and can range from explicit traumatic events to subtle, chronic stressors.
Historical Trauma and Attachment Wounds
Your early life experiences significantly shape your nervous system’s default responses. If you experienced inconsistent caregiving, emotional neglect, or abuse as a child, your nervous system may have learned that shutdown was the safest option. When a child’s cries for help are repeatedly unmet or met with hostility, their system learns that activation (fight or flight) is dangerous, and immobility becomes the primary survival strategy. This early programming can create a nervous system that is highly sensitive to perceived abandonment, rejection, or overwhelming situations, even in adulthood. These experiences lay down neural pathways that predispose you to enter shutdown when similar internal or external cues are present.
Chronic Stress and Overwhelm
Modern life often presents a relentless onslaught of demands, deadlines, and information. When your sympathetic nervous system is continuously activated by stress, without adequate periods of rest and recovery, it can eventually exhaust itself. Imagine a car engine constantly redlining; eventually, it will seize up. This sustained state of hyperarousal can lead to a compensatory shutdown, where the DVC kicks in to conserve resources and prevent burnout. This is not necessarily about a single traumatic event, but rather a cumulative build-up of unaddressed stress. This can include demanding work environments, financial insecurity, relational conflicts, or ongoing health issues.
Perceived Lack of Agency or Control
A core element of the shutdown response is the brain’s assessment that an escape or fight response is futile. If you frequently find yourself in situations where you feel trapped, powerless, or without control over your circumstances, your nervous system is more likely to activate the DVC. This can range from oppressive workplaces to abusive relationships, or even chronic illness where you feel your body is betraying you. The feeling of helplessness is a potent trigger, signaling to your ancient brain that the best course of action is to “play dead.”
Shifting Out of Dorsal Vagal Shutdown
The process of moving out of shutdown involves carefully and incrementally reactivating your nervous system towards a state of ventral vagal engagement. This is not a race; pushing too hard can paradoxically reinforce the shutdown or trigger a sympathetic (fight/flight) response. Think of it like coaxing a shy animal out of hiding – it requires patience, gentleness, and creating a sense of safety.
Gentle Movement and Proprioception
One of the most effective ways to begin shifting out of shutdown is through gentle, conscious movement. Because shutdown involves a feeling of disconnection from the body, re-establishing this connection is vital. Proprioception – your body’s sense of its position and movement in space – is key.
- Slow, Deliberate Movements: Avoid sudden, jarring movements. Instead, focus on slow, intentional actions. Wriggle your toes and fingers, gently rotate your ankles and wrists. Notice the feeling of your clothes on your skin, the temperature of the air. This helps to bring your attention back into your body.
- Grounding Techniques: Place your feet firmly on the floor and feel their connection to the ground. Press your hands together or against a solid surface. Try a “body scan” meditation, where you systematically bring awareness to different parts of your body.
- Stretching: Gentle stretching can release latent tension and stimulate sensory feedback. Focus on areas that tend to hold tension, such as the neck, shoulders, and hips. Avoid overstretching, which can feel threatening to an already fragile system.
- Walking: A slow, mindful walk, especially in nature, can be incredibly restorative. Focus on the rhythm of your steps, the sensations in your feet, and the sights and sounds around you. This bilateral movement can help regulate the nervous system.
Sensory Input to Anchor in the Present
When you are in shutdown, your world can feel muffled and unreal. Introducing gentle, regulating sensory input can help to bring you back into the present moment and signal safety to your nervous system.
- Temperature Regulation: Applying a warm compress to your chest or belly can be comforting and signals safety. Conversely, splashes of cool water on your face or wrists can be gently stimulating. Experiment to see what feels most regulating for you.
- Pleasant Scents: Olfactory input is directly linked to the limbic system, which processes emotions and memory. Gentle, calming scents such as lavender, chamomile, or sandalwood can be grounding. Avoid overpowering scents that might trigger overwhelm.
- Calming Sounds: Listen to soft, instrumental music, nature sounds (like rain or gentle waves), or binaural beats designed for relaxation. Avoid loud, chaotic, or jarring sounds, which can amplify the feeling of threat.
- Visual Anchors: Focus on a visually pleasing object in your environment – a plant, a piece of art, or a comforting photograph. Notice its colors, textures, and details. This helps to anchor your attention and interrupt the dissociative haze.
- Taste: Slowly savor a small piece of food or a comforting drink. Pay attention to its texture, temperature, and flavor. This mindful consumption can be a powerful way to engage your senses and return to the present.
Cultivating Ventral Vagal Engagement
While exiting shutdown is crucial, the long-term goal is to build resilience and increase your capacity for ventral vagal engagement. This means developing the ability to feel safe, connected, and present, even amidst life’s challenges.
Co-Regulation and Safe Connection
Humans are social creatures, and our nervous systems are designed to regulate each other. Co-regulation, the process of two or more individuals regulating each other’s emotional states, is a powerful tool for healing.
- Connecting with Safe Others: Seek out individuals who make you feel genuinely safe, understood, and seen. This could be a trusted friend, family member, therapist, or even a pet. Engage in gentle conversation, share a comforting silence, or simply be in their presence. The presence of a regulated nervous system can subtly encourage your own to regulate.
- Mindful Touch: If comfortable, safe, and consensual, gentle touch can be profoundly regulating. A hand on your arm, a comforting hug, or even holding hands can communicate safety and connection. Ensure the touch is welcome and feels nurturing, not intrusive.
- Eye Contact: Sustained, soft eye contact with a trusted individual can activate the ventral vagal system, supporting connection and feelings of safety. However, if eye contact feels threatening, start with brief glances or focus on other cues of presence.
Practices for Self-Regulation
Beyond external connection, developing internal resources for self-regulation is essential. These practices train your nervous system to access the ventral vagal state more readily.
- Mindful Breathing: Slow, deep, diaphragmatic breathing is a direct pathway to activating the ventral vagus. Practice inhaling slowly through your nose, letting your belly expand, and exhaling even more slowly through your mouth. Try techniques like “box breathing” (inhale for 4, hold for 4, exhale for 4, hold for 4) or extending your exhale.
- Vagal Toning Exercises: Specific exercises can “tone” your vagus nerve, increasing its resilience. These include humming, singing, chanting, gargling, and even laughing. These activities stimulate the muscles in the throat and soft palate, which are innervated by the vagus nerve.
- Mindfulness and Self-Compassion: Practicing mindfulness means paying attention to the present moment without judgment. This helps you to notice when you are slipping into shutdown and to gently guide yourself back. Self-compassion involves treating yourself with kindness and understanding, especially when you are struggling. This internal kindness can be a powerful antidote to the harsh self-criticism that often accompanies shutdown.
- Nature Immersion: Spending time in nature has been shown to reduce stress and promote nervous system regulation. Engage your senses – the smell of pine, the sound of birds, the feel of the earth beneath your feet.
Understanding the dorsal vagal shutdown response is crucial for those seeking to heal from trauma and stress-related disorders. One effective approach involves exploring various therapeutic techniques that can help individuals reconnect with their bodies and emotions. For more insights on this topic, you can read a related article that discusses practical strategies for overcoming this response and fostering resilience. By implementing these strategies, individuals may find a path toward healing and improved emotional regulation. To learn more, visit this helpful resource.
Professional Support and Long-Term Healing
| Metric | Description | Measurement Method | Typical Range | Notes |
|---|---|---|---|---|
| Heart Rate Variability (HRV) | Indicator of autonomic nervous system balance and vagal tone | ECG or wearable heart rate monitors | High HRV indicates better vagal regulation | Improvement suggests recovery from dorsal vagal shutdown |
| Respiratory Rate | Breathing rate reflecting parasympathetic activation | Respiratory sensors or manual counting | 12-20 breaths per minute (normal adult range) | Slower, deep breathing supports vagal activation |
| Skin Conductance Level (SCL) | Measures sympathetic nervous system arousal | Electrodermal activity sensors | Lower SCL indicates reduced stress response | Decrease may reflect healing from shutdown state |
| Self-Reported Calmness | Subjective rating of emotional state | Standardized questionnaires or visual analog scales | Scale 1-10, higher scores indicate calmness | Improvement correlates with dorsal vagal recovery |
| Social Engagement Scale | Assessment of social interaction and connection | Behavioral observation or self-report | Higher scores indicate better social engagement | Increased engagement suggests vagal system healing |
While self-help strategies are invaluable, addressing chronic dorsal vagal shutdown, especially if rooted in trauma, often benefits from professional guidance. A skilled therapist can provide a safe container and specific techniques to navigate this complex terrain.
Trauma-Informed Therapy Approaches
Several therapeutic modalities are particularly effective in helping individuals process trauma and regulate their nervous systems.
- Somatic Experiencing (SE): Developed by Peter Levine, SE focuses on helping you track physical sensations in your body and safely release stored trauma energy. It’s about slowly completing the “fight or flight” responses that were interrupted during a traumatic event, without re-traumatizing you. You learn to pendulate between uncomfortable and comfortable sensations, gradually increasing your capacity to tolerate activation without shutting down.
- Polyvagal-Informed Therapy: Therapists trained in Polyvagal Theory explicitly work with the nuances of your autonomic nervous system. They help you identify your nervous system states, understand their triggers, and develop strategies to move towards ventral vagal safety. This approach often involves psychoeducation, body-based exercises, and building social engagement skills.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR is an evidence-based therapy that helps process distressing memories and reduce their emotional impact. While not exclusively body-focused, it can help desensitize the nervous system to triggers that lead to shutdown.
- Internal Family Systems (IFS): IFS views the psyche as composed of various “parts,” including those that might feel frozen or shut down. It helps you to understand and compassionately work with these parts, integrating them into a more cohesive self.
- Neurofeedback: This is a non-invasive process that measures brainwaves and provides real-time feedback, helping you to train your brain to regulate itself more effectively. It can be particularly helpful for chronic dysregulation.
Building Resilience and Preventing Relapse
Healing is not a one-time event but an ongoing process. Building resilience means equipping yourself with tools and habits that promote nervous system regulation and prevent you from slipping back into chronic shutdown.
- Establish Routines: Predictable routines, especially around sleep, meals, and self-care, provide a sense of safety and stability to your nervous system.
- Boundary Setting: Learn to identify and communicate your boundaries effectively. Saying “no” to overwhelming demands protects your energy and signals to your nervous system that you have agency.
- Mindful Reflection: Regularly check in with your body and emotions. Ask yourself: “How do I feel right now? What does my nervous system need?” This self-awareness is critical for early intervention.
- Connect with Purpose: Engaging in activities that bring you meaning and purpose can be deeply regulating and foster a sense of vitality, counteracting the emptiness of shutdown.
- Sustained Self-Care: Prioritize activities that genuinely nourish you – whether it’s creative pursuits, spending time in nature, spiritual practices, or simply quiet contemplation. Self-care is not a luxury, but a fundamental aspect of nervous system hygiene.
- Community and Support: Maintian healthy relationships and foster a sense of belonging. Social support is a powerful buffer against stress and a vital resource for navigating life’s challenges.
Healing the dorsal vagal shutdown response is a journey of re-inhabiting your body, reclaiming your agency, and rebuilding your capacity for connection and joy. It requires patience, persistence, and a deep commitment to self-compassion. By understanding the mechanisms of shutdown, recognizing its triggers, and implementing targeted strategies for regulation and resilience, you can gradually move towards a life characterized by presence, vitality, and genuine safety.
WARNING: Your “Peace” Is Actually A Trauma Response
FAQs
What is the dorsal vagal shutdown response?
The dorsal vagal shutdown response is a physiological reaction controlled by the dorsal branch of the vagus nerve, part of the parasympathetic nervous system. It is often triggered by extreme stress or trauma, leading to a state of immobilization, dissociation, or shutdown as a survival mechanism.
What causes the dorsal vagal shutdown response?
This response is typically caused by overwhelming stress, trauma, or perceived life-threatening situations. When the body perceives that fight or flight is not possible, the dorsal vagal system activates to conserve energy and protect vital functions by reducing heart rate, blood pressure, and metabolic activity.
How can one recognize signs of dorsal vagal shutdown?
Signs may include feelings of numbness, dissociation, extreme fatigue, low energy, difficulty engaging socially, slowed heart rate, shallow breathing, and a sense of disconnection from the environment or self.
What are common approaches to healing the dorsal vagal shutdown response?
Healing approaches often involve trauma-informed therapies such as somatic experiencing, mindfulness, breathwork, gentle movement, and grounding techniques. These methods aim to safely re-engage the nervous system, restore regulation, and promote a sense of safety and connection.
Is professional help necessary for healing from dorsal vagal shutdown?
While some individuals may benefit from self-help techniques, professional guidance from therapists trained in trauma and nervous system regulation is often recommended. They can provide tailored interventions and support to effectively address and heal the shutdown response.




