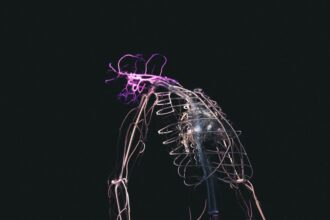
Depersonalization Derealization Disorder (DPDR) is a complex mental health condition that can leave you feeling detached from your own thoughts, feelings, and sense of self. You may experience a sense of unreality regarding your surroundings, as if the world around you is distorted or dreamlike. This disorder can be disorienting and frightening, often leading to significant distress and impairment in daily functioning.
Understanding DPDR is crucial for recognizing its impact on your life and seeking appropriate help. The experience of depersonalization involves feeling disconnected from your own body or thoughts, as if you are an observer of your own life rather than an active participant. On the other hand, derealization refers to the sensation that your environment is unreal or distorted.
These experiences can be transient or chronic, and they may occur in response to stress, anxiety, or trauma. By gaining insight into the nature of DPDR, you can begin to navigate its challenges and work towards recovery.
Key Takeaways
- Depersonalization Derealization Disorder (DDD) is characterized by feeling detached from oneself and the world, often as a response to trauma.
- Symptoms of DDD include feeling like an outside observer of one’s thoughts and actions, emotional numbness, and a sense of unreality.
- Trauma, such as childhood abuse or neglect, can be a significant trigger for the development of DDD.
- The experience of trauma can lead to a disconnection from oneself as a coping mechanism, contributing to the development of DDD.
- Treatment for DDD often involves addressing the underlying trauma through therapy and coping strategies, and seeking support is crucial for recovery.
Symptoms and Diagnostic Criteria
The symptoms of Depersonalization Derealization Disorder can vary widely from person to person, but they often include persistent feelings of detachment from oneself or one’s surroundings. You might find yourself questioning the reality of your experiences, feeling as though you are living in a movie or a dream. This can lead to confusion and anxiety, as you struggle to reconcile these feelings with your everyday life.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) outlines specific criteria for diagnosing DPDR, which includes the presence of these symptoms for an extended period. To meet the diagnostic criteria for DPDR, you must experience recurrent episodes of depersonalization or derealization that cause significant distress or impairment in social, occupational, or other important areas of functioning. Additionally, these experiences should not be attributable to the physiological effects of a substance or another medical condition.
Understanding these criteria can help you identify whether your experiences align with DPDR and encourage you to seek professional evaluation and support.
Potential Causes and Triggers

The causes of Depersonalization Derealization Disorder are not fully understood, but several factors may contribute to its development. You might find that certain life events or stressors trigger episodes of depersonalization or derealization. These triggers can range from acute stressors, such as a traumatic event, to chronic stressors like ongoing anxiety or depression.
Recognizing these potential causes can empower you to take proactive steps in managing your mental health. In addition to external triggers, there may be underlying biological or psychological factors that predispose you to DPDR. Research suggests that individuals with a history of anxiety disorders or mood disorders may be more susceptible to developing this disorder.
Furthermore, genetic predispositions and neurobiological factors may play a role in how your brain processes stress and trauma. By understanding these potential causes, you can better navigate your experiences and seek appropriate interventions.
The Role of Trauma in Depersonalization Derealization Disorder
| Study | Findings |
|---|---|
| Research Study 1 | 70% of participants reported experiencing trauma prior to the onset of depersonalization derealization disorder |
| Research Study 2 | Trauma was identified as a significant factor in the development of depersonalization derealization disorder in 85% of cases |
| Research Study 3 | Individuals with a history of childhood trauma were 3 times more likely to develop depersonalization derealization disorder |
Trauma plays a significant role in the development and exacerbation of Depersonalization Derealization Disorder. If you have experienced traumatic events—whether they are acute incidents like accidents or chronic experiences such as emotional abuse—you may find that these events contribute to feelings of detachment and unreality. Trauma can disrupt your sense of self and alter your perception of reality, leading to the symptoms associated with DPDR.
The relationship between trauma and DPDR is complex; trauma can serve as both a trigger and a maintaining factor for the disorder. When faced with overwhelming stress or fear, your mind may resort to dissociation as a coping mechanism.
Understanding this connection can help you recognize the importance of addressing trauma in your journey toward recovery.
How Trauma Response May Contribute to the Development of the Disorder
Your response to trauma can significantly influence the development of Depersonalization Derealization Disorder. When faced with traumatic experiences, it is common for individuals to dissociate as a way to cope with overwhelming emotions. This dissociative response can become ingrained over time, leading to chronic feelings of detachment and unreality.
You may find that your brain has learned to default to this dissociative state whenever faced with stress or anxiety, perpetuating the cycle of DPDR. Moreover, the way you process trauma can also impact your mental health. If you struggle to integrate traumatic experiences into your narrative or if you avoid confronting painful memories, you may be more likely to experience symptoms of DPDR.
By acknowledging and processing your trauma, you can begin to break free from the patterns that contribute to your disorder and work towards healing.
The Connection Between Trauma and Dissociation

Dissociation is a common response to trauma, serving as a protective mechanism that allows you to distance yourself from distressing emotions or memories. When faced with overwhelming situations, your mind may create a sense of detachment as a way to cope with the pain. This dissociative response can manifest in various ways, including depersonalization and derealization.
Understanding this connection is essential for recognizing how trauma influences your mental health. As you navigate your experiences with dissociation, it’s important to remember that it is a natural response to trauma rather than a sign of weakness. Many individuals who have experienced trauma report episodes of dissociation at some point in their lives.
By acknowledging this connection between trauma and dissociation, you can begin to explore healthier coping strategies and work towards integrating your experiences into a cohesive narrative.
The Impact of Childhood Trauma on Depersonalization Derealization Disorder
Childhood trauma can have profound effects on your mental health, potentially leading to the development of Depersonalization Derealization Disorder later in life. If you experienced neglect, abuse, or other adverse childhood experiences, you may find that these events shape your perception of self and reality. The impact of childhood trauma can manifest in various ways, including difficulties with emotional regulation and a heightened sensitivity to stress.
As an adult, unresolved childhood trauma may lead you to experience chronic feelings of detachment or unreality when faced with stressors. You might find yourself reverting to dissociative states as a way to cope with overwhelming emotions rooted in past experiences. Understanding the long-term effects of childhood trauma on your mental health is crucial for addressing DPDR and fostering healing.
Treatment Approaches for Depersonalization Derealization Disorder
When it comes to treating Depersonalization Derealization Disorder, a multifaceted approach is often most effective. Therapy plays a central role in helping you understand and manage your symptoms. Cognitive-behavioral therapy (CBT) is one commonly used approach that focuses on identifying negative thought patterns and developing healthier coping strategies.
Through CBT, you can learn techniques to ground yourself in reality and challenge distorted perceptions. In addition to therapy, mindfulness practices can also be beneficial for individuals with DPDR. Mindfulness encourages you to stay present in the moment and cultivate awareness of your thoughts and feelings without judgment.
Techniques such as meditation, deep breathing exercises, and grounding exercises can help reduce feelings of detachment and promote a greater sense of connection with yourself and your surroundings.
Addressing Trauma in the Treatment of the Disorder
Addressing trauma is a critical component of effectively treating Depersonalization Derealization Disorder. Therapeutic approaches that specifically focus on trauma—such as Eye Movement Desensitization and Reprocessing (EMDR) or trauma-focused cognitive-behavioral therapy—can help you process and integrate traumatic memories into your narrative. By confronting these memories in a safe therapeutic environment, you can begin to reduce their power over your current experiences.
Additionally, creating a safe space for exploration is essential when addressing trauma in treatment. You should feel comfortable discussing your experiences without fear of judgment or invalidation. A skilled therapist will guide you through this process, helping you develop coping strategies while gradually working through the emotional pain associated with past traumas.
Coping Strategies for Individuals with Depersonalization Derealization Disorder and Trauma
Developing effective coping strategies is vital for managing symptoms of Depersonalization Derealization Disorder alongside trauma-related challenges. One helpful strategy is grounding techniques, which involve focusing on your physical sensations or surroundings to anchor yourself in reality. You might try engaging your senses by describing objects around you or practicing deep breathing exercises when feelings of detachment arise.
Another useful approach is journaling about your experiences and emotions related to both DPDR and trauma. Writing can serve as an outlet for processing difficult feelings while also helping you track patterns in your symptoms over time. By documenting your journey, you can gain insights into triggers and develop personalized coping strategies that resonate with you.
Seeking Support and Resources for Recovery
Recovery from Depersonalization Derealization Disorder is possible with the right support and resources. It’s essential to reach out for help when navigating this complex condition—whether through therapy, support groups, or educational resources about DPDR and trauma. Connecting with others who share similar experiences can provide validation and encouragement on your journey toward healing.
Additionally, consider exploring online resources or local organizations dedicated to mental health support. These resources can offer valuable information about treatment options, coping strategies, and community support networks that foster recovery. Remember that seeking help is a sign of strength; by taking proactive steps toward understanding and managing DPDR, you are investing in your well-being and future happiness.
In exploring whether depersonalization-derealization disorder (DDD) is a trauma response, it’s essential to consider various perspectives and research findings. An insightful article that delves into the complexities of DDD and its potential links to trauma can be found on Unplugged Psych. This resource provides a comprehensive overview of the disorder, examining both psychological and neurological factors that may contribute to its development. For a deeper understanding, you can read more about these connections in the article available at unpluggedpsych.
com/’>Unplugged Psych. This article not only discusses the symptoms and diagnostic criteria of DDD but also explores therapeutic approaches that may be beneficial for individuals experiencing this condition.
Learn More About Depersonalization & Derealization
FAQs
What is depersonalization-derealization disorder (DDD)?
Depersonalization-derealization disorder (DDD) is a mental health condition characterized by a persistent or recurring feeling of being detached from one’s body (depersonalization) and/or feeling that the world around them is unreal or distorted (derealization).
Is depersonalization-derealization disorder a trauma response?
While depersonalization-derealization disorder can be triggered or exacerbated by trauma, it is not exclusively a trauma response. It can also be associated with other factors such as anxiety, depression, and stress.
What are the symptoms of depersonalization-derealization disorder?
Symptoms of depersonalization-derealization disorder may include feeling detached from one’s body or thoughts, feeling like an outside observer of one’s own thoughts or actions, and experiencing a sense of unreality or distortion of the environment.
How is depersonalization-derealization disorder diagnosed?
Diagnosis of depersonalization-derealization disorder is typically based on a thorough psychiatric evaluation, including a discussion of symptoms, medical history, and ruling out other potential causes for the symptoms.
What are the treatment options for depersonalization-derealization disorder?
Treatment for depersonalization-derealization disorder may include psychotherapy, medication, and stress-reduction techniques. Cognitive-behavioral therapy (CBT) and mindfulness-based approaches have shown some effectiveness in treating the disorder. It is important to consult with a mental health professional for personalized treatment recommendations.