Your brain is an extraordinary organ, intricately designed to protect you from harm. One of its most vital functions is its ability to detect and respond to pain, a mechanism that serves as a warning system for potential injury or illness. This protective mechanism is not merely a reflex; it involves complex neural pathways and processes that allow you to react swiftly to threats.
When you touch something hot or experience a sudden jolt, your brain springs into action, signaling your body to withdraw from the source of pain. This immediate response is crucial for your survival, as it helps prevent further damage. Understanding how your brain processes pain can provide insight into why you experience discomfort in certain situations and how you can manage it effectively.
The brain’s protective mechanism is not just about the sensation of pain; it encompasses a wide range of emotional and psychological responses that influence how you perceive and react to pain. By delving deeper into this fascinating subject, you can gain a better understanding of your own experiences with pain and the various factors that contribute to your pain perception.
Key Takeaways
- The brain has protective mechanisms in place to help avoid pain and ensure survival.
- Pain signals are processed in the brain through a complex network of neurons and neurotransmitters.
- The amygdala plays a key role in pain avoidance by processing emotional responses to pain.
- Neurotransmitters like endorphins and serotonin play a role in modulating pain perception and response.
- Emotions, previous experiences, and adaptive behaviors all influence how the brain perceives and avoids pain.
How the Brain Processes Pain Signals
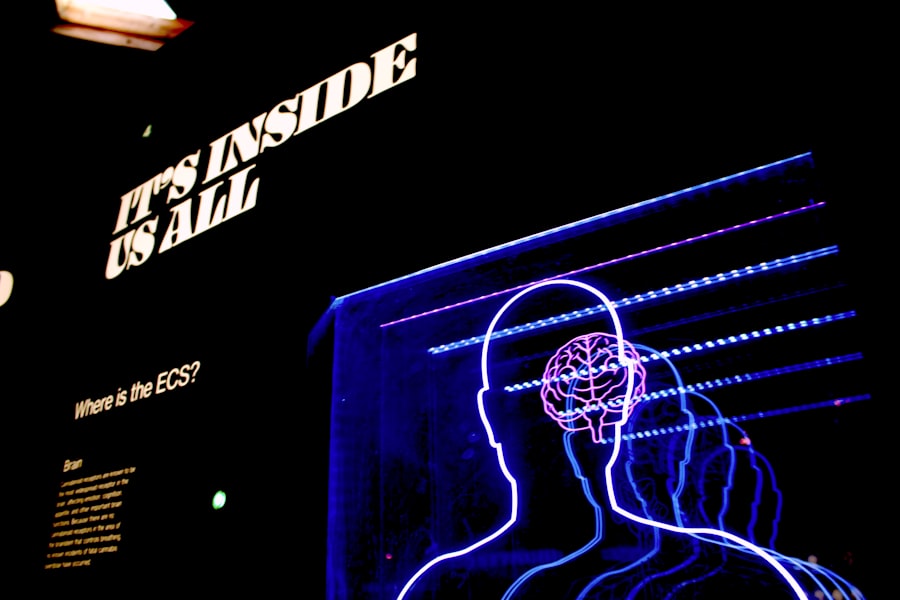
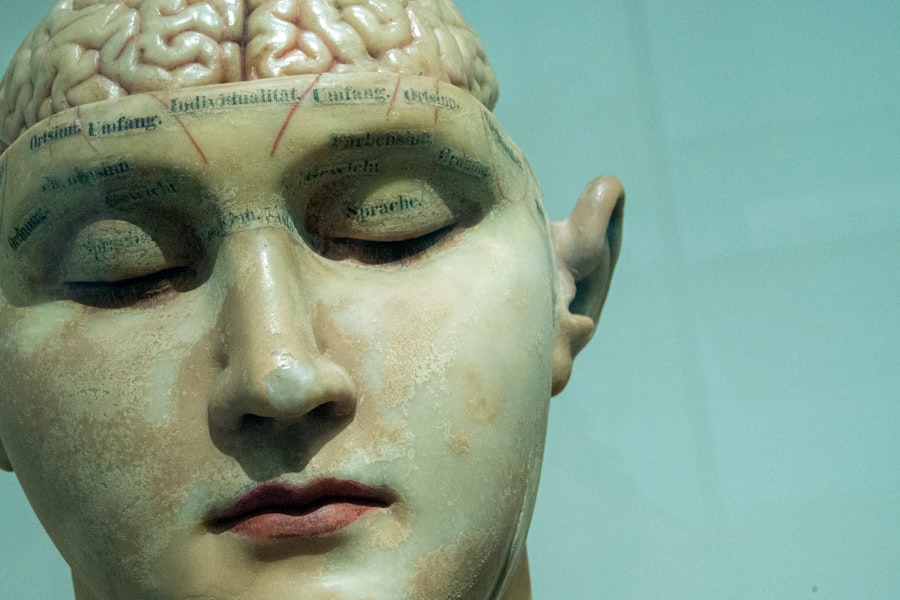
When you experience pain, your body sends signals through specialized nerve fibers to your spinal cord and then to your brain. This process begins with nociceptors, which are sensory receptors that detect harmful stimuli. Once activated, these receptors transmit electrical signals along nerve pathways to the spinal cord, where they are relayed to the brain.
The thalamus acts as a relay station, directing these signals to various regions of the brain for further processing. This intricate network ensures that you are aware of the pain and can respond appropriately. As the signals reach the brain, they are interpreted in different areas, including the somatosensory cortex, which helps you identify the location and intensity of the pain.
Meanwhile, the anterior cingulate cortex and insula are involved in processing the emotional aspects of pain, allowing you to experience not just the physical sensation but also the emotional weight it carries. This multifaceted approach to pain processing highlights how your brain integrates sensory information with emotional responses, ultimately shaping your overall experience of pain.
The Role of the Amygdala in Pain Avoidance
The amygdala plays a crucial role in how you respond to pain, particularly in terms of avoidance behavior. This almond-shaped structure in your brain is primarily associated with emotional processing and fear responses. When you experience pain, the amygdala becomes activated, triggering a cascade of reactions that can lead to heightened anxiety and fear surrounding potential future pain.
This response is essential for survival, as it encourages you to avoid situations that may lead to injury or discomfort. Your amygdala’s involvement in pain avoidance can also lead to learned behaviors. For instance, if you touch a hot stove and feel intense pain, your amygdala will remember this experience, making you more likely to avoid similar situations in the future.
This learned avoidance can be beneficial in protecting you from harm; however, it can also lead to excessive fear and anxiety about pain, which may hinder your ability to engage in everyday activities. Understanding the role of the amygdala in pain avoidance can help you recognize when fear may be influencing your behavior and how to address it.
Neurotransmitters and Pain Modulation
| Neurotransmitter | Function | Role in Pain Modulation |
|---|---|---|
| Glutamate | Excitatory neurotransmitter | Involved in the transmission of pain signals |
| GABA (Gamma-aminobutyric acid) | Inhibitory neurotransmitter | Regulates pain perception and reduces pain sensation |
| Endorphins | Natural painkillers | Bind to opioid receptors to reduce pain perception |
| Substance P | Neuropeptide | Enhances pain transmission and sensitivity |
Neurotransmitters are chemical messengers that play a significant role in how your brain modulates pain signals. Various neurotransmitters, such as substance P, glutamate, and endorphins, interact with receptors in your nervous system to either amplify or dampen pain sensations. For example, when you experience acute pain, substance P is released, enhancing the transmission of pain signals to your brain.
Conversely, endorphins act as natural pain relievers by binding to opioid receptors and inhibiting the perception of pain. The balance between these neurotransmitters is crucial for effective pain management. If your body produces too much of certain neurotransmitters, you may experience heightened sensitivity to pain, known as hyperalgesia.
On the other hand, insufficient levels of endorphins can lead to increased discomfort and difficulty coping with pain. By understanding how neurotransmitters influence your pain experience, you can explore strategies for modulating these chemicals through lifestyle changes or medical interventions.
The Influence of Emotions on Pain Perception
Your emotional state significantly impacts how you perceive and respond to pain. Research has shown that negative emotions such as anxiety, depression, and stress can amplify your experience of pain, making it feel more intense and difficult to manage. When you’re feeling anxious or stressed, your body releases stress hormones like cortisol, which can heighten sensitivity to pain and create a cycle of discomfort that is hard to break.
Conversely, positive emotions and a sense of well-being can help mitigate pain perception. Engaging in activities that bring you joy or practicing mindfulness techniques can promote relaxation and reduce stress levels, ultimately leading to a more manageable experience of pain. By recognizing the connection between your emotions and pain perception, you can take proactive steps to cultivate a more positive emotional environment that supports your overall well-being.
The Impact of Previous Experiences on Pain Avoidance
Your past experiences with pain play a significant role in shaping your current responses and avoidance behaviors. If you’ve had traumatic experiences related to pain—such as surgery or injury—your brain may develop a heightened sensitivity to similar situations in the future. This phenomenon is known as conditioned pain modulation, where previous painful experiences create a learned response that influences how you perceive new instances of discomfort.
For instance, if you’ve had a negative experience at the dentist’s office, you may feel anxious about future dental visits even if they are routine and less painful than before. This learned avoidance can lead to increased fear and anxiety surrounding dental care, potentially resulting in neglecting necessary treatments. By understanding how previous experiences shape your current perceptions of pain, you can work towards reframing those memories and reducing their impact on your present behavior.
Adaptive Behaviors and Pain Avoidance
Adaptive behaviors are essential for managing pain effectively and ensuring your overall well-being. When faced with potential sources of discomfort, your brain encourages you to adopt behaviors that minimize risk and promote healing. For example, if you’ve recently injured yourself, your body may instinctively guide you to rest and avoid activities that could exacerbate the injury.
These adaptive behaviors are crucial for recovery and help prevent further harm. However, it’s important to strike a balance between adaptive behaviors and avoidance behaviors that may limit your quality of life. While it’s natural to want to avoid situations that cause discomfort, excessive avoidance can lead to decreased physical activity and social withdrawal.
By recognizing when avoidance becomes counterproductive, you can work towards developing healthier coping strategies that allow you to navigate discomfort without sacrificing your quality of life.
The Role of Chronic Pain in Altered Pain Processing
Chronic pain presents a unique challenge when it comes to understanding how your brain processes pain signals. Unlike acute pain, which serves as a protective mechanism for immediate threats, chronic pain persists long after an injury has healed or without any identifiable cause. This ongoing discomfort can lead to alterations in how your brain processes pain signals over time.
Your nervous system may become sensitized, resulting in heightened sensitivity even in response to non-painful stimuli—a phenomenon known as allodynia. The experience of chronic pain can also lead to changes in brain structure and function. Research has shown that individuals with chronic pain may exhibit alterations in areas responsible for emotional regulation and sensory processing.
These changes can create a feedback loop where increased sensitivity leads to heightened emotional distress, further exacerbating the perception of pain. Understanding the complexities of chronic pain processing is essential for developing effective treatment strategies that address both physical symptoms and emotional well-being.
The Connection Between Pain Avoidance and Survival
Pain avoidance is deeply rooted in evolutionary biology; it serves as a fundamental survival mechanism that has been honed over millennia.
This instinctual response has been passed down through generations, ensuring that individuals who were more adept at avoiding danger were more likely to survive and reproduce.
In modern society, while many threats have changed or diminished, the instinctual drive for pain avoidance remains strong within you. This drive influences not only how you respond to physical threats but also how you navigate social situations and emotional challenges. Recognizing this connection between pain avoidance and survival can help you appreciate the biological underpinnings of your responses while also encouraging you to develop healthier coping mechanisms that allow for growth beyond mere survival.
The Influence of Social and Cultural Factors on Pain Avoidance
Your social environment plays a significant role in shaping how you perceive and respond to pain. Cultural beliefs about pain can influence whether you view it as something to be endured silently or expressed openly. In some cultures, expressing discomfort may be seen as a sign of weakness, leading individuals to suppress their feelings rather than seek help or support.
Conversely, other cultures may encourage open discussions about pain and suffering, fostering an environment where individuals feel comfortable seeking assistance. Social support networks also play a crucial role in how you cope with pain avoidance behaviors. Friends and family members can provide encouragement and understanding during difficult times, helping you navigate challenges related to discomfort more effectively.
By recognizing the impact of social and cultural factors on your experiences with pain, you can work towards creating an environment that supports healthy coping strategies while fostering open communication about discomfort.
Strategies for Managing Pain Avoidance in Chronic Pain Conditions
Managing pain avoidance in chronic conditions requires a multifaceted approach that addresses both physical symptoms and emotional well-being. One effective strategy is cognitive-behavioral therapy (CBT), which focuses on identifying negative thought patterns related to pain and replacing them with healthier perspectives. By reframing your thoughts about discomfort, you can reduce anxiety surrounding potential triggers and develop more adaptive coping mechanisms.
Additionally, engaging in regular physical activity tailored to your abilities can help combat avoidance behaviors while promoting overall health. Exercise releases endorphins—natural mood lifters—that can alleviate feelings of discomfort while improving physical function over time. Mindfulness practices such as meditation or yoga can also be beneficial by fostering relaxation and reducing stress levels associated with chronic pain.
In conclusion, understanding the complex interplay between your brain’s protective mechanisms, emotional responses, past experiences, social influences, and coping strategies is essential for effectively managing pain avoidance behaviors in chronic conditions. By exploring these factors holistically, you can develop personalized strategies that empower you to navigate discomfort while enhancing your overall quality of life.
The human brain has evolved intricate mechanisms to avoid pain, which is crucial for survival. This instinctive response is explored in greater detail in the article on Unplugged Psych, where the psychological and neurological underpinnings of pain avoidance are discussed. For more insights, you can read the full article [here](https://www.unpluggedpsych.com/sample-page/). Understanding these processes can help us develop better coping strategies and therapeutic approaches to manage pain effectively.
WATCH THIS! Spiritual Bypassing Is Your Brains Favorite Lie
FAQs
What is pain?
Pain is a complex and unpleasant sensory and emotional experience that is associated with actual or potential tissue damage. It serves as a protective mechanism to alert the body to potential harm.
How does the brain process pain?
The brain processes pain through a complex network of neurons and neurotransmitters. When the body experiences pain, specialized nerve cells called nociceptors send signals to the brain, which then interprets and processes the information.
Why does the brain avoid pain?
The brain avoids pain as a protective mechanism to prevent further harm to the body. It does so by triggering reflex actions, such as pulling away from a hot surface, and by releasing natural pain-relieving chemicals, such as endorphins.
What are some ways the brain avoids pain?
The brain can avoid pain through various mechanisms, including the release of endorphins, the activation of the body’s natural pain modulation system, and the processing of pain signals in a way that minimizes the perception of pain.
Can the brain become desensitized to pain?
Yes, the brain can become desensitized to pain through repeated exposure to painful stimuli, a phenomenon known as pain adaptation. This can occur in certain chronic pain conditions or with the use of certain pain management techniques.




