Understanding the Neuroscience of Anxiety
Anxiety, a ubiquitous human experience, often manifests as a distressing mental and physiological state characterized by apprehension, worry, and fear. While considered a normal adaptive response in certain situations, such as encountering a genuine threat, chronic or excessive anxiety can significantly impair your daily functioning and overall well-being. To truly grasp the pervasive nature of anxiety, you must delve into its neurobiological underpinnings, exploring the intricate neural circuits and biochemical pathways that orchestrate its emergence and persistence. This article will guide you through the fundamental neuroscience of anxiety, providing you with a foundational understanding of how your brain processes and perpetuates this complex emotion.
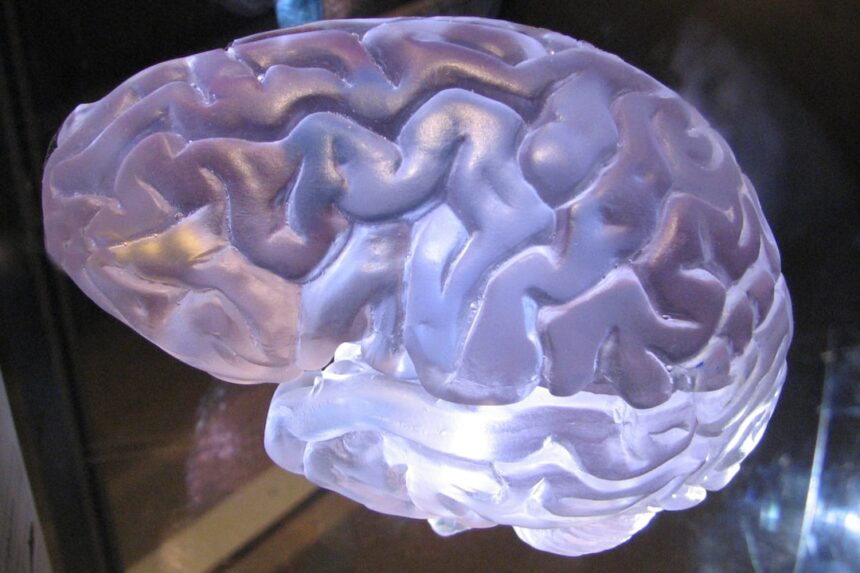
At the core of your brain’s fear and anxiety response lies the amygdala, a small, almond-shaped structure nestled deep within the temporal lobe. Think of your amygdala as your brain’s sophisticated alarm system, constantly scanning your environment for potential threats.
How the Amygdala Processes Threat Information
When you encounter a potentially dangerous stimulus, sensory information, whether visual, auditory, or tactile, travels rapidly to your thalamus. From there, this information takes two distinct pathways: a “low road” and a “high road.”
The Low Road: A Shortcut to Fear
The low road is a direct, fast-acting pathway from the thalamus straight to your amygdala. This route allows for exceptionally rapid threat detection, almost like a reflex. For instance, if you unexpectedly encounter a snake in your path, your amygdala receives this information instantaneously and initiates a fear response before your conscious mind has fully registered what you’re seeing. This rapid processing is crucial for survival, enabling you to react to immediate dangers without the delay of full cognitive analysis. You are essentially reacting before you even consciously know why.
The High Road: Adding Context and Nuance
Simultaneously, the sensory information also travels along the “high road,” a more circuitous route that involves the sensory cortex. Here, the information undergoes more detailed processing and interpretation. Your prefrontal cortex and hippocampus, for example, contribute contextual information, allowing you to assess whether the perceived threat is genuine or benign. If, after further analysis, your cortex determines the “snake” was merely a garden hose, it sends inhibitory signals to your amygdala, dampening the fear response. This intricate interplay between the low and high roads highlights the brain’s remarkable capacity for both rapid threat detection and nuanced contextual evaluation.
The Amygdala’s Role in Memory and Emotional Learning
The amygdala is not merely a detector of immediate threats; it also plays a critical role in the formation and retrieval of emotional memories, particularly those associated with fear. When you experience a frightening event, your amygdala strengthens the neural connections related to that experience, making it more likely that you will react with fear in similar situations in the future. This process, known as fear conditioning, is a powerful learning mechanism that can be both adaptive and maladaptive. For example, if you were bitten by a dog as a child, your amygdala might associate all dogs with danger, leading to a generalized fear. Understanding this mechanism is vital as it provides insight into how anxiety can become ingrained and persistent.
For those interested in the neuroscience of anxiety, a fascinating article can be found at Unplugged Psych, which delves into the brain mechanisms underlying anxiety disorders and their implications for treatment. This resource provides valuable insights into how neurobiology influences anxiety responses and offers a comprehensive overview of current research in the field. You can read more about it by visiting Unplugged Psych.
The Prefrontal Cortex: The Brain’s Brake System
While the amygdala acts as your brain’s alarm, your prefrontal cortex (PFC), particularly the ventromedial prefrontal cortex (vmPFC) and dorsolateral prefrontal cortex (dlPFC), functions as the executive control center, providing a crucial “brake” on your anxiety response.
Regulating Emotional Responses
Your PFC is responsible for higher-order cognitive functions such as planning, decision-making, working memory, and emotional regulation. In the context of anxiety, the vmPFC plays a pivotal role in inhibiting the amygdala’s activity. It does this by sending direct inhibitory projections to the amygdala, effectively dampening its alarm signals. When you consciously evaluate a situation and determine that it is not genuinely threatening, your vmPFC steps in to override the amygdala’s initial fear response.
The Impaired Brake in Anxiety Disorders
In individuals with anxiety disorders, this inhibitory control exerted by the PFC often appears to be compromised. Imagine a car where the accelerator (amygdala) is stuck, and the brakes (PFC) are weakened. This imbalance leads to an overactive amygdala and insufficient top-down regulation, resulting in persistent and excessive anxiety. Neuroimaging studies have consistently shown reduced activity in the vmPFC and increased activity in the amygdala in individuals suffering from various anxiety disorders. This observation underlines the critical importance of a healthy and well-functioning PFC in maintaining emotional balance.
Cognitive Reappraisal and Exposure Therapy
Understanding the role of the PFC provides a neurobiological basis for therapeutic interventions like cognitive behavioral therapy (CBT), particularly cognitive reappraisal and exposure therapy. In cognitive reappraisal, you actively challenge and reframe negative thoughts and interpretations of anxiety-provoking situations. This process engages your PFC, strengthening its ability to override maladaptive amygdala responses. Similarly, exposure therapy, where you gradually and safely confront feared objects or situations, helps your PFC learn that these stimuli are not actually dangerous, thereby weakening the fear associations stored in the amygdala and reinforcing inhibitory control. You are, in essence, retraining your brain’s brake system.
Neurotransmitters: The Brain’s Chemical Messengers

Your brain orchestrates its complex functions through a sophisticated network of chemical messengers known as neurotransmitters. Several key neurotransmitters play crucial roles in modulating anxiety, acting like finely tuned instruments in a complex symphony.
Gamma-Aminobutyric Acid (GABA): The Brain’s Natural Tranquilizer
GABA is the primary inhibitory neurotransmitter in your central nervous system. Think of GABA as your brain’s natural tranquilizer; it calms neuronal activity, effectively reducing excitability and promoting relaxation. When GABA binds to its receptors, it decreases the likelihood that a neuron will fire, thereby quieting excessive neural chatter.
GABAergic Dysregulation in Anxiety
Dysregulation in the GABAergic system is strongly implicated in anxiety disorders. Individuals with anxiety often exhibit reduced GABA levels or impaired GABA receptor function. This deficiency means that the brain’s natural braking system is less effective, leading to heightened neuronal excitability and increased anxiety. Many anxiolytic medications, such as benzodiazepines, work by enhancing GABA’s effects, thereby promoting a calming influence on the brain. However, long-term use of such medications carries risks, demonstrating the delicate balance you must maintain within this system.
Serotonin: Mood Regulator and Anxiety Modulator
Serotonin, a monoamine neurotransmitter, is widely known for its role in mood regulation, sleep, appetite, and learning. It also plays a significant role in modulating anxiety. Serotonin neurons project to various brain regions involved in anxiety, including the amygdala, hippocampus, and prefrontal cortex, influencing their activity.
Imbalances in Serotonin and Anxiety
An imbalance in serotonin levels, particularly a deficiency, has been linked to increased anxiety and depression. Selective serotonin reuptake inhibitors (SSRIs), a common class of antidepressant and anxiolytic medications, work by increasing serotonin levels in the synaptic cleft, thereby enhancing serotonin signaling and improving mood and reducing anxiety over time. However, the precise mechanisms by which serotonin influences anxiety are complex and involve multiple receptor subtypes, making it a nuanced area of research.
Norepinephrine: The Fight-or-Flight Neurotransmitter
Norepinephrine, also known as noradrenaline, is both a neurotransmitter and a hormone involved in your body’s “fight-or-flight” response. It prepares your body for action by increasing heart rate, blood pressure, and alertness.
Norepinephrine Overactivity in Anxiety
While a certain level of norepinephrine is necessary for alertness and focus, overactivity in the noradrenergic system is a hallmark of many anxiety disorders, particularly panic disorder. When you experience excessive norepinephrine release, you might feel a surge of physical symptoms associated with anxiety, such as a pounding heart, shortness of breath, and sweating. Beta-blockers, a class of medication used to treat physical symptoms of anxiety, work by blocking the effects of norepinephrine on certain receptors, thereby reducing the physiological manifestations of arousal. This highlights the tight connection between your mental state and your body’s physical responses.
The Hippocampus: Context and Memory in Anxiety
Your hippocampus, another crucial brain structure located in the temporal lobe, is intimately involved in memory formation, spatial navigation, and distinguishing between safe and threatening contexts. Its role in anxiety is multifaceted.
Contextual Fear Conditioning
The hippocampus helps you learn and remember the context in which fearful events occurred. For instance, if you experience a traumatic event in a specific location, your hippocampus will associate that location with fear. This allows you to avoid similar dangerous situations in the future. However, in anxiety disorders, the hippocampus can become overactive or dysregulated, leading to difficulties in distinguishing between safe and dangerous contexts. You may, for example, feel anxious in a neutral environment because your hippocampus has generalized a past fear response to that setting, even if objectively there is no threat.
Overgeneralization of Fear in Anxiety
One of the key issues in chronic anxiety is the overgeneralization of fear. Your hippocampus, in conjunction with the amygdala, struggles to accurately differentiate between genuinely dangerous and safe situations. This means that a stimulus that once posed a threat might, even when presented in a safe context, still trigger an anxiety response. Imagine a smoke detector that goes off for burnt toast as often as it does for a full-blown fire; this is analogous to how your brain might misinterpret harmless cues as threats in an anxious state. Impaired hippocampal function contributes to this overgeneralization, making it difficult for you to unlearn fear associations.
Impact of Stress on the Hippocampus
Chronic stress, a significant contributor to anxiety, can have detrimental effects on your hippocampus. Prolonged exposure to cortisol, a stress hormone, can lead to atrophy of hippocampal neurons and impaired neurogenesis (the growth of new neurons). This damage can further compromise your ability to regulate fear and anxiety, creating a vicious cycle where stress exacerbates anxiety, and anxiety, in turn, contributes to hippocampal dysfunction. Protecting your brain from chronic stress is therefore not just about mental well-being, but also about maintaining the structural integrity of crucial brain regions.
Recent advancements in the neuroscience of anxiety have shed light on the intricate mechanisms underlying this common mental health condition. Researchers are increasingly exploring how brain structures and neurochemical pathways contribute to anxiety disorders, leading to potential new treatment options. For those interested in a deeper understanding of these developments, a related article can be found at Unplugged Psych, which discusses the latest findings in this fascinating field. This exploration not only enhances our knowledge but also paves the way for innovative therapeutic approaches.
The Hypothalamic-Pituitary-Adrenal (HPA) Axis: The Stress Response System
| Metric | Description | Typical Findings in Anxiety | Measurement Method |
|---|---|---|---|
| Amygdala Activation | Level of activity in the amygdala, a brain region involved in fear processing | Increased activation in response to threat-related stimuli | fMRI, PET scans |
| Prefrontal Cortex (PFC) Regulation | Activity in the PFC, responsible for executive control and emotion regulation | Reduced activity or connectivity with amygdala, leading to impaired regulation | fMRI, EEG |
| Hippocampal Volume | Size of the hippocampus, involved in memory and contextual processing | Often reduced volume in chronic anxiety disorders | MRI volumetric analysis |
| Cortisol Levels | Concentration of cortisol, a stress hormone linked to anxiety | Elevated baseline or reactive cortisol levels | Saliva, blood, or urine assays |
| Heart Rate Variability (HRV) | Variation in time intervals between heartbeats, indicating autonomic nervous system balance | Lower HRV indicating higher anxiety and stress | ECG monitoring |
| GABA Concentration | Levels of gamma-aminobutyric acid, the main inhibitory neurotransmitter | Reduced GABA levels associated with increased anxiety | MRS (Magnetic Resonance Spectroscopy) |
| Serotonin Transporter Availability | Density of serotonin transporters affecting serotonin signaling | Altered transporter availability linked to anxiety symptoms | SPECT, PET imaging |
The HPA axis is your body’s central stress response system, a complex neuroendocrine pathway that plays a critical role in mediating your physiological and behavioral reactions to stress and anxiety. Think of it as a master control panel for managing stress.
The Cascade of Stress Hormones
When you perceive a threat or experience stress, your hypothalamus, located at the base of your brain, releases corticotropin-releasing hormone (CRH). CRH then signals your pituitary gland to release adrenocorticotropic hormone (ACTH). ACTH, in turn, travels through your bloodstream to your adrenal glands, which sit atop your kidneys. The adrenal glands then release cortisol, your primary stress hormone.
Cortisol: The Body’s Stress Amplifier
Cortisol has wide-ranging effects throughout your body, mobilizing energy reserves, suppressing non-essential functions, and enhancing your sensory perception to help you cope with the perceived threat. While acute cortisol release is adaptive and protective, chronic elevation of cortisol, often seen in individuals with chronic anxiety, can have profound and detrimental effects on your physical and mental health. This sustained activation acts like an always-on siren, keeping your body in a perpetual state of alert.
Dysregulation of the HPA Axis in Anxiety
In individuals with chronic anxiety disorders, the HPA axis often becomes dysregulated. This can manifest as either hyperactivation (excessive release of cortisol) or blunted cortisol responses, depending on the specific anxiety disorder and individual factors. Both scenarios indicate an imbalanced stress response system that is no longer functioning optimally. This dysregulation is thought to contribute to the persistent physiological symptoms of anxiety, such as increased heart rate, muscle tension, and sleep disturbances. Furthermore, chronic cortisol exposure can negatively impact brain regions involved in emotional regulation, such as the hippocampus and prefrontal cortex, thus perpetuating the anxiety cycle.
Feedback Loops and Anxiety
The HPA axis operates on a negative feedback loop. Under normal circumstances, elevated cortisol levels signal your hypothalamus and pituitary gland to reduce the release of CRH and ACTH, thereby dampening the stress response. However, in chronic anxiety, this feedback loop can become impaired, leading to a sustained and amplified stress response. This impaired feedback mechanism is like a thermostat that fails to turn off the heating, leading to an unnecessarily overheated system. Understanding this feedback loop is vital for appreciating how anxiety disorders can maintain themselves over long periods.
In conclusion, understanding the neuroscience of anxiety requires a journey into the intricate workings of your brain and its chemical messengers. While specific brain regions like the amygdala, prefrontal cortex, and hippocampus act as key players, it is the dynamic interplay between these structures, modulated by neurotransmitters like GABA, serotonin, and norepinephrine, and orchestrated by the HPA axis, that ultimately shapes your experience of anxiety. By appreciating these complex neurobiological mechanisms, you can gain a deeper insight into the origins and persistence of anxiety, paving the way for more targeted and effective therapeutic interventions. You are not simply experiencing an abstract emotion; you are witnessing the complex dance of your own brain.
FAQs
What is the neuroscience of anxiety?
The neuroscience of anxiety studies how brain structures, neural circuits, and biochemical processes contribute to the experience and regulation of anxiety. It explores how different brain regions, such as the amygdala and prefrontal cortex, interact to produce anxiety responses.
Which brain areas are primarily involved in anxiety?
Key brain areas involved in anxiety include the amygdala, which processes fear and threat detection; the prefrontal cortex, which regulates emotional responses; the hippocampus, which is involved in memory and context; and the hypothalamus, which controls physiological stress responses.
How do neurotransmitters affect anxiety?
Neurotransmitters like gamma-aminobutyric acid (GABA), serotonin, norepinephrine, and dopamine play crucial roles in anxiety. For example, GABA generally inhibits neural activity and reduces anxiety, while imbalances in serotonin and norepinephrine systems are linked to increased anxiety symptoms.
Can neuroscience explain why some people are more prone to anxiety?
Yes, neuroscience research suggests that genetic factors, brain structure differences, and variations in neural circuitry can make some individuals more susceptible to anxiety. Early life stress and environmental factors also influence brain development and anxiety vulnerability.
How does understanding the neuroscience of anxiety help in treatment?
Understanding the neural mechanisms of anxiety aids in developing targeted treatments such as medications that modulate neurotransmitter systems and therapies like cognitive-behavioral therapy (CBT) that can alter brain activity patterns. It also helps in identifying biomarkers for better diagnosis and personalized interventions.