You’re experiencing a spike in Depersonalization-Derealization Disorder (DPDR) symptoms, and you suspect sleep deprivation is a significant contributor. This is a common and understandable occurrence. DPDR, a dissociative disorder characterized by feelings of detachment from oneself (depersonalization) and one’s surroundings (derealization), can be amplified by a lack of adequate sleep. When your brain is starved of rest, its coping mechanisms can falter, making you more susceptible to these disorienting experiences. This article aims to provide you with practical, factual strategies to manage these sleep deprivation-induced spikes, helping you regain a sense of groundedness when the veil of dissociation feels particularly thick.
The relationship between sleep and DPDR is complex and often cyclical. When you’re sleep-deprived, your brain’s ability to regulate emotions, process sensory input, and maintain a stable sense of self is compromised. This can act like a faulty circuit breaker, causing the delicate balance that underpins your conscious experience to overload.
The Neurological Impact of Sleep Deprivation
During sleep, your brain undergoes crucial restorative processes. The hippocampus, vital for memory consolidation and emotional regulation, is actively engaged. The prefrontal cortex, responsible for executive functions like decision-making, impulse control, and self-awareness, also benefits from sleep. When these areas are deprived of their necessary downtime, their functionality can be impaired.
Disrupted Neurotransmitter Balance
Adequate sleep is essential for the balanced production and regulation of neurotransmitters, the chemical messengers that transmit signals between nerve cells. Sleep deprivation can disrupt the levels and activity of neurotransmitters such as serotonin, dopamine, and norepinephrine, which play roles in mood, arousal, and perception. Imbalances in these systems can contribute to feelings of disconnection and unreality.
Impaired Emotional Processing
REM (Rapid Eye Movement) sleep, in particular, is thought to be critical for processing emotional experiences. Insufficient REM sleep can leave you with a backlog of unprocessed emotions, making you more reactive to stress and more prone to anxious or dissociative states. Think of it as trying to clear a crowded inbox without taking the time to sort and respond; the sheer volume can become overwhelming.
The Vicious Cycle of Sleep and DPDR
For individuals with DPDR, sleep disturbances are frequently reported. This can manifest as insomnia, fragmented sleep, or difficulty falling asleep. The anxiety and distress associated with DPDR itself can further exacerbate sleep problems, creating a detrimental feedback loop. When you’re worried about experiencing dissociation, the very act of trying to sleep can become a source of stress, making it even harder to achieve restful sleep. This then feeds back into your DPDR symptoms, potentially leading to spikes.
If you’re struggling with sleep deprivation spikes in depersonalization-derealization disorder (DPDR), you may find it helpful to explore additional resources that address this issue. One such article discusses effective strategies for managing sleep disturbances and their impact on DPDR symptoms. You can read more about these techniques and tips for improving your sleep quality by visiting this link: here.
Proactive Sleep Hygiene: Your First Line of Defense
Establishing and maintaining robust sleep hygiene is paramount for buffering against sleep deprivation-induced DPDR spikes. This involves creating an environment and adopting habits that promote consistent, high-quality sleep. Consider these practices as building a strong fortress around your well-being, making it more resilient to external pressures like lack of sleep.
Creating a Conducive Sleep Environment
Your bedroom should be a sanctuary for sleep, free from distractions and optimized for rest.
Optimize Light Exposure
Darkness signals to your brain that it’s time to wind down and produce melatonin, the sleep-promoting hormone.
Minimize Blue Light Before Bed
Electronic devices like smartphones, tablets, and computers emit blue light, which can suppress melatonin production and interfere with your natural sleep-wake cycle. Aim to power down these devices at least one to two hours before bedtime. If you must use them, consider using blue light filtering glasses or night mode settings.
Ensure Complete Darkness
Use blackout curtains or blinds to block out any external light sources. Even small amounts of light can disrupt sleep.
Temperature Regulation
A slightly cooler room temperature is generally more conducive to sleep. Experiment to find the optimal temperature for you, typically between 60-67°F (15-19°C).
Noise Reduction
A quiet environment is essential for uninterrupted sleep. If you live in a noisy area, consider using earplugs or a white noise machine to mask disruptive sounds. White noise can act as a gentle tide, washing over distracting noises and creating a calm auditory landscape.
Establishing a Consistent Sleep Schedule
Your body thrives on regularity, and a consistent sleep schedule is one of the most powerful tools for regulating your internal clock.
Weekday and Weekend Consistency
While life can be unpredictable, strive to maintain a similar bedtime and wake-up time, even on weekends. Significant deviations can throw off your circadian rhythm, making it harder to fall asleep and wake up naturally. Imagine your circadian rhythm as a finely tuned instrument; even small deviations in tuning can affect the overall harmony.
The Importance of Wake-Up Time
Your wake-up time is arguably more important than your bedtime for setting your biological clock. Waking up at the same time each day helps anchor your sleep cycle.
Developing a Relaxing Bedtime Routine
A pre-sleep routine signals to your body and mind that it’s time to transition from an active day to a restful night.
Wind-Down Activities
Engage in calming activities that help you de-stress and relax. This could include:
Gentle Stretching or Yoga
Releasing physical tension can help prepare your body for sleep.
Reading a Physical Book
Opt for a physical book rather than an e-reader to avoid blue light exposure. Choose something engaging but not overly stimulating.
Taking a Warm Bath or Shower
The rise and subsequent fall in body temperature after a warm bath can promote sleepiness.
Meditation or Deep Breathing Exercises
These practices can help calm your nervous system and quiet a racing mind. Focus on the sensation of your breath, a steady anchor in the storm of thoughts.
Avoid Stimulants and Heavy Meals
Refrain from consuming caffeine or alcohol in the hours leading up to bedtime. Similarly, avoid large, heavy meals close to sleep, as they can cause digestive discomfort.
Addressing Immediate Sleep Deprivation Spikes

When you find yourself in the throes of a DPDR spike, and you know sleep deprivation is a contributing factor, immediate, focused strategies are necessary. These are your emergency tools, designed to bring you back from the brink.
Prioritizing Rest, Even When Difficult
When sleep deprivation has already taken hold and DPDR symptoms are escalating, your primary goal is to get some form of rest, even if it’s not ideal sleep.
Power Naps: A Strategic Respite
Short, strategically timed naps can be incredibly beneficial.
Duration Matters
Aim for naps of 20-30 minutes, which can provide a restorative boost without leading to grogginess or interfering with nighttime sleep. Longer naps can sometimes deepen sleep inertia, making you feel more disoriented.
Timing is Key
Avoid napping too close to your usual bedtime, as this can make it harder to fall asleep later. Early afternoon is often the optimal time for a power nap.
Creating a “Rest Hour”
If you can’t fall asleep, dedicate a specific hour to simply resting in a quiet, dark environment. Even if you’re not sleeping, this period of enforced stillness can be restorative. Close your eyes, focus on your breath, and allow your body to relax without pressure to sleep.
Mindful Interventions During a Spike
When DPDR symptoms are at their peak due to sleep deprivation, cultivating mindfulness can help you anchor yourself in the present moment.
Grounding Techniques
These techniques focus on connecting you to your physical senses and the immediate environment.
Sensory Awareness
Engage your senses deliberately. What do you see, hear, smell, taste, and feel? As you hold a cool object, focus on its texture and temperature.
The “5-4-3-2-1” Method
Identify five things you can see, four things you can touch, three things you can hear, two things you can smell, and one thing you can taste. This mental checklist pulls you out of your internal landscape and into the external world.
Deep Breathing Exercises
Controlled breathing can have a calming effect on the nervous system.
Diaphragmatic Breathing
Focus on breathing deeply into your belly, allowing your abdomen to rise with each inhale. This type of breathing activates the parasympathetic nervous system, promoting relaxation. Your breath is an ever-present anchor; even when the waters of dissociation feel turbulent, returning to your breath can offer stability.
Avoiding Maladaptive Coping Mechanisms
In moments of distress, it’s tempting to resort to behaviors that offer temporary relief but ultimately worsen the situation.
Limiting Excessive Reassurance Seeking
Constantly seeking validation that you are “real” or “okay” can paradoxically reinforce the underlying anxiety and disconnection.
Avoiding Rumination and Overthinking
When sleep-deprived, your mind can become a runaway train of negative thoughts. Try to gently redirect your attention when you notice yourself getting caught in these thought loops.
Long-Term Strategies for Sleep Improvement

Beyond immediate crisis management, building a foundation of consistent, quality sleep is your most potent weapon against DPDR spikes. These are the ongoing practices that fortify your defenses.
Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is a highly effective, evidence-based treatment for chronic insomnia. It addresses the thoughts and behaviors that interfere with sleep.
Understanding Sleep Psychology
CBT-I educates you about the mechanisms of sleep and how various factors can disrupt it. This knowledge dispels misconceptions and empowers you with effective strategies.
Behavioral Interventions
This can include:
Stimulus Control Therapy
This involves strengthening the association between your bed and sleep, and eliminating behaviors that weaken this link. For example, if you can’t sleep after 20 minutes, you get out of bed and only return when you feel sleepy. The goal is to break the cycle of associating your bed with frustration and wakefulness.
Sleep Restriction Therapy
This involves temporarily reducing your time in bed to consolidate your sleep and increase your sleep drive. While it might sound counterintuitive to restrict sleep further, it can lead to more efficient and restorative sleep over time.
Addressing Underlying Mental Health Conditions
DPDR often co-occurs with other mental health conditions such as anxiety disorders, depression, or trauma-related disorders. These conditions can significantly impact sleep patterns.
Seeking Professional Help
If you suspect an underlying condition is contributing to your sleep problems and DPDR, consulting a therapist or psychiatrist is crucial. They can provide a comprehensive assessment and tailor a treatment plan to your specific needs. This might involve medication, psychotherapy, or a combination of both.
Medication Management
In some cases, medication may be prescribed to address underlying anxiety or depression, which in turn can improve sleep and reduce DPDR symptoms. Your healthcare provider will carefully weigh the benefits and risks of any medication.
Lifestyle Adjustments for Enhanced Sleep Quality
Beyond the immediate sleep hygiene practices, certain lifestyle choices can have a profound impact on your overall sleep architecture.
Regular Physical Activity
Consistent exercise can significantly improve sleep quality. However, it’s important to time your workouts appropriately.
Avoid Intense Exercise Close to Bedtime
Vigorous physical activity too close to sleep can be stimulating and make it harder to fall asleep. Aim to complete your workouts at least a few hours before bedtime.
Moderate Exercise for Sleep Benefits
Gentle forms of exercise like walking or swimming can be done closer to bedtime and may even promote relaxation.
Balanced Nutrition
Your diet plays a role in your sleep patterns.
Avoid Heavy Meals and Sugary Snacks Late at Night
These can disrupt digestion and blood sugar levels, interfering with sleep.
Consider Sleep-Promoting Foods
Certain foods, like those rich in magnesium or tryptophan, may support sleep. Examples include almonds, walnuts, dairy products, and poultry.
Sleep deprivation can significantly exacerbate symptoms of depersonalization-derealization disorder (DPDR), making it crucial to find effective coping strategies. One helpful resource is an article that discusses various techniques for managing sleep deprivation spikes in individuals experiencing DPDR. By implementing these strategies, you can improve your overall well-being and reduce the intensity of your symptoms. For more insights on this topic, you can read the article on Unplugged Psych, which offers valuable information on navigating the challenges of sleep and mental health.
Recognizing Triggers and Building Resilience
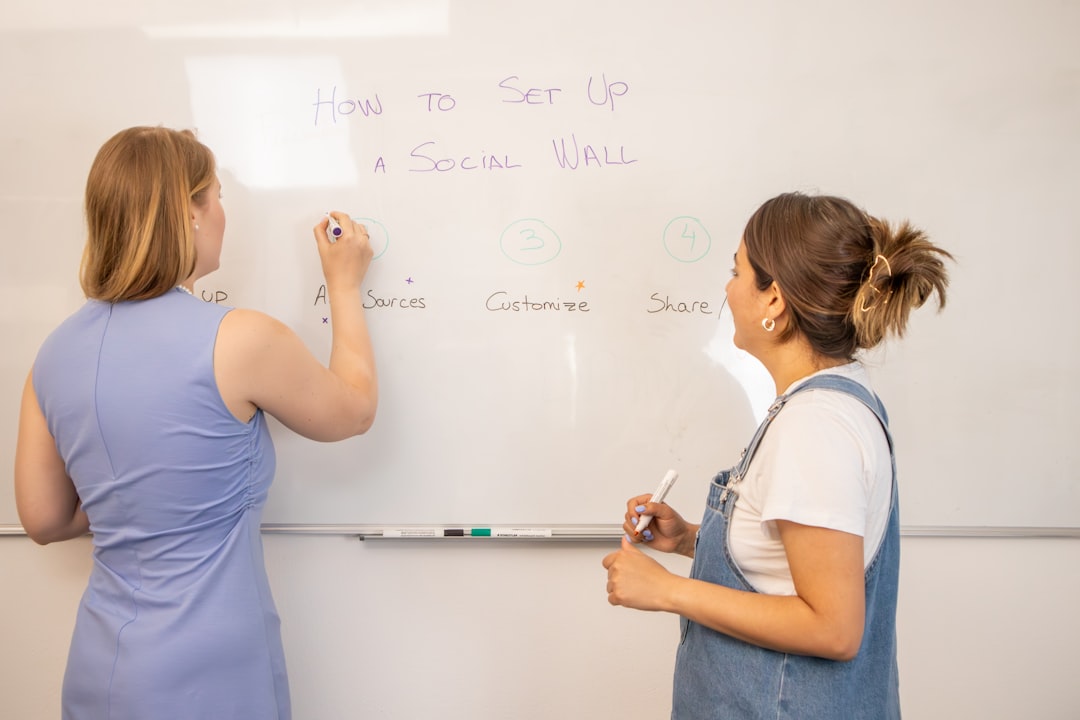
| Strategy | Description | Effectiveness | Notes |
|---|---|---|---|
| Maintain a Consistent Sleep Schedule | Go to bed and wake up at the same time daily to regulate circadian rhythm. | High | Helps reduce DPDR symptoms by improving overall sleep quality. |
| Practice Relaxation Techniques | Use meditation, deep breathing, or progressive muscle relaxation before sleep. | Moderate to High | Reduces anxiety that can worsen DPDR during sleep deprivation. |
| Limit Stimulants | Avoid caffeine, nicotine, and other stimulants especially in the afternoon/evening. | Moderate | Prevents interference with falling asleep and reduces DPDR spikes. |
| Short Naps | Take 20-30 minute naps to alleviate acute sleep deprivation without disrupting nighttime sleep. | Moderate | Helps reduce immediate DPDR symptoms but avoid long naps. |
| Physical Activity | Engage in regular moderate exercise to improve sleep quality and reduce stress. | Moderate | Avoid intense exercise close to bedtime. |
| Seek Professional Help | Consult a healthcare provider or therapist for persistent DPDR and sleep issues. | High | May include cognitive behavioral therapy or medication. |
| Limit Screen Time Before Bed | Reduce exposure to blue light from phones, computers, and TVs at least 1 hour before sleep. | Moderate | Improves melatonin production and sleep onset. |
Understanding what triggers your sleep deprivation spikes is a critical step in managing them. It’s about building a mental armor against the inevitable ebb and flow of life.
Identifying Personal Sleep Deprivation Triggers
Everyone’s vulnerability to sleep deprivation differs. What may push one person into a DPDR spike might not affect another as severely.
Stress and Anxiety
High levels of stress and anxiety are notorious sleep disruptors. When faced with stressful situations, your mind can race, making sleep elusive.
Illness and Physical Discomfort
When you’re unwell or experiencing physical pain, sleep can become a luxury. This can cascade into sleep deprivation and exacerbate DPDR.
Changes in Routine
Travel, shift work, or significant life events can disrupt your established sleep patterns, making you more susceptible to spikes.
Developing a Personalized Action Plan
Once you’ve identified your triggers, you can develop a personalized plan to mitigate their impact.
Pre-emptive Sleep Strategies
When you anticipate a period of increased stress or a disruption to your routine, be extra diligent with your sleep hygiene in the days leading up to it. This proactive approach can help you build a buffer of rest.
Troubleshooting During a Spike
Have a clear, pre-defined set of strategies you can implement immediately when you notice a spike occurring. This might involve a specific grounding exercise, a short meditation, or a power nap. Knowing what to do can reduce the panic and feeling of helplessness.
Building a Support System
You don’t have to navigate these challenges alone. A strong support system can provide emotional comfort and practical assistance.
Open Communication with Loved Ones
Share your experiences with trusted friends or family members. Explaining DPDR and the impact of sleep deprivation can foster understanding and provide you with a listening ear when you need it most.
Connecting with Support Groups
Online or in-person support groups for DPDR can be invaluable. Connecting with others who understand your struggles can reduce feelings of isolation and offer shared coping strategies.
Seeking Professional Guidance for Persistent Issues
While self-management strategies are powerful, some individuals require professional intervention to effectively manage sleep deprivation-induced DPDR spikes.
When to Consult a Healthcare Professional
If your sleep problems are chronic, significantly impacting your daily functioning, or if your DPDR symptoms are severe and persistent, it’s essential to seek professional help.
Signs You May Need Professional Support
- Persistent insomnia: You struggle to fall asleep or stay asleep most nights.
- Excessive daytime sleepiness: You feel drowsy and fatigued throughout the day, despite attempting to sleep.
- Significant impact on daily life: Your DPDR symptoms and sleep difficulties are interfering with your work, relationships, or ability to perform basic tasks.
- Escalating anxiety or depression: Your symptoms are worsening, or you’re experiencing new or more intense mental health concerns.
The Role of Therapists and Sleep Specialists
A multidisciplinary approach often yields the best results.
Therapists Specializing in Dissociative Disorders
Therapists trained in treating DPDR can help you understand the underlying mechanisms and develop effective coping strategies. They can also address any co-occurring mental health conditions.
Sleep Specialists and Clinics
If sleep hygiene alone isn’t sufficient, a sleep specialist can conduct a formal sleep study (polysomnography) to diagnose any underlying sleep disorders, such as sleep apnea or restless legs syndrome, which could be contributing to your sleep deprivation.
The Importance of a Holistic Approach
Managing sleep deprivation spikes in DPDR is a journey that often requires patience and persistence. By implementing these strategies, you are actively reclaiming control over your sleep and, consequently, over your sense of self and reality. Remember, you are not defined by your dissociative experiences; you are a resilient individual capable of navigating these challenges with the right tools and support. Your journey back to a stable sense of self, even in the face of sleep deprivation’s disruptive influence, is a testament to your inner strength.
THE DPDR EXIT PLAN: WARNING: Your Brain Is Stuck In “Safety Mode”
FAQs
What is DPDR and how is it related to sleep deprivation?
Depersonalization-Derealization Disorder (DPDR) is a dissociative condition characterized by feelings of detachment from oneself or the environment. Sleep deprivation can exacerbate DPDR symptoms by increasing stress and impairing cognitive function, leading to more intense episodes.
How does sleep deprivation trigger spikes in DPDR symptoms?
Lack of sleep disrupts normal brain function, affecting areas responsible for perception and emotional regulation. This disruption can intensify feelings of unreality and detachment, causing spikes in DPDR symptoms.
What are effective strategies to manage sleep deprivation when experiencing DPDR?
Effective strategies include maintaining a consistent sleep schedule, creating a relaxing bedtime routine, avoiding caffeine and electronic devices before sleep, practicing relaxation techniques, and seeking professional help if sleep issues persist.
Can improving sleep quality reduce the frequency or intensity of DPDR episodes?
Yes, improving sleep quality can help stabilize brain function and reduce stress, which may decrease the frequency and intensity of DPDR episodes. Adequate rest supports emotional regulation and cognitive clarity.
When should someone with DPDR seek medical advice regarding sleep problems?
If sleep deprivation is frequent, severe, or significantly worsens DPDR symptoms, it is important to consult a healthcare professional. They can assess for underlying sleep disorders and recommend appropriate treatments or therapies.