The Polyvagal Theory, developed by Dr. Stephen Porges, offers a compelling framework for understanding the intricate connection between your physiological states, your emotions, and your behavior. It expands beyond the traditional fight-or-flight paradigm, introducing a third, often misunderstood, survival strategy: the freeze response. This article will guide you through the polyvagal theory’s explanation of freeze, elucidating its biological underpinnings, its manifestation in your daily life, and pathways to navigating its often debilitating effects.
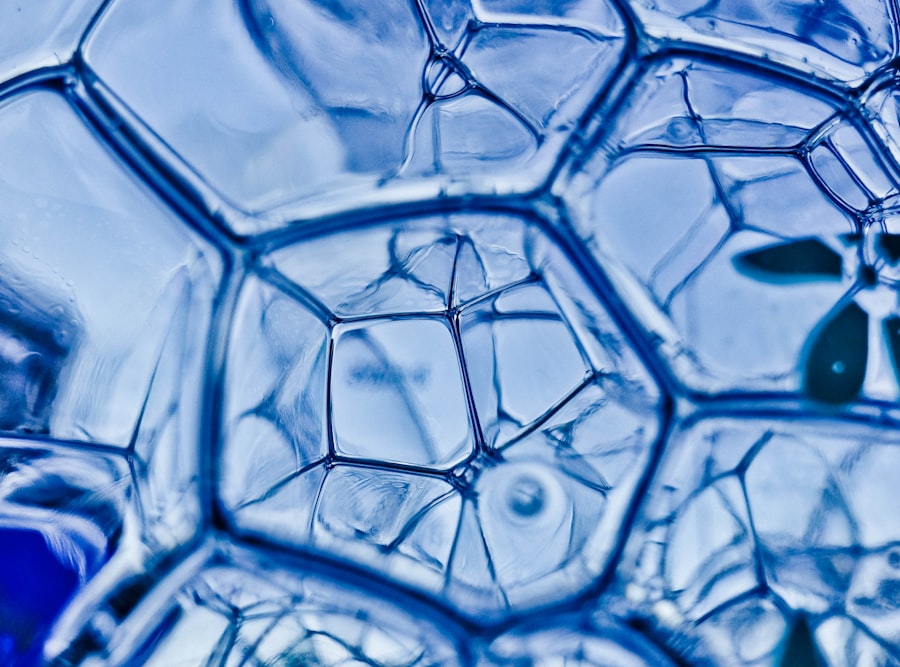
To grasp the freeze response fully, you must first understand the core tenets of Polyvagal Theory. This theory posits that your autonomic nervous system (ANS), rather than being a simple two-lane highway of sympathetic and parasympathetic activation, is organized hierarchically into three distinct neural circuits. Each circuit is associated with specific physiological and behavioral responses, evolving over millennia to optimize your survival in an ever-changing environment.
The Autonomic Nervous System: More Than Just Fight or Flight
You likely recognize the sympathetic nervous system as the system responsible for your “fight or flight” reactions. When faced with a perceived threat, your heart rate accelerates, your muscles tense, and your senses sharpen, preparing you for immediate action. Conversely, the parasympathetic nervous system is typically associated with “rest and digest” – lowering your heart rate, promoting digestion, and fostering a sense of calm. However, Polyvagal Theory reveals a more nuanced picture.
The Vagus Nerve: A Bifurcated Pathway
The vagus nerve, a major component of your parasympathetic nervous system, is central to Polyvagal Theory. Dr. Porges identified two distinct branches of the vagus nerve, each with unique functions and evolutionary origins.
The Myelinated Ventral Vagal Complex (VVC)
This is the most recently evolved branch of the vagus nerve and is unique to mammals. The VVC originates in the brainstem and innervates your facial muscles, your heart, and your lungs above the diaphragm. It is crucial for social engagement, emotional regulation, and fostering a sense of safety. When your VVC is actively engaged, you experience a sense of connection, warmth, and ease. You can engage in reciprocal communication, your voice has a comforting tone, and your facial expressions are welcoming. Think of this as your “social connection” system.
The Unmyelinated Dorsal Vagal Complex (DVC)
This is the oldest and most evolutionarily conserved branch of the vagus nerve. The DVC originates in the brainstem and primarily innervates your organs below the diaphragm, including your stomach, intestines, and bladder. Its primary function is immobilization, or “playing dead,” as a last-resort survival strategy. When your DVC is dominant, your metabolic rate drops significantly, your heart rate slows dramatically, and you may experience a sense of dissociation or numbness. This is your “shutdown” system.
Polyvagal theory offers a fascinating insight into the freeze response, highlighting how our autonomic nervous system influences our reactions to stress and trauma. For a deeper understanding of this concept, you can explore the related article that delves into the intricacies of the freeze response and its implications for mental health. To read more, visit this article.
The Ladder of Autonomic States
Imagine your autonomic nervous system as a ladder, with each rung representing a distinct physiological state. Your body constantly climbs and descends this ladder in response to perceived safety or threat.
The Top Rung: Social Engagement (Ventral Vagal)
At the top of the ladder, you find the state of social engagement, governed by your Ventral Vagal Complex. In this state, you feel safe, connected, and present. Your ability to communicate effectively, empathize with others, and experience joy is at its peak. This is your optimal state for learning, growth, and flourishing.
The Middle Rung: Mobilization (Sympathetic)
Just below social engagement is the state of mobilization, driven by your sympathetic nervous system. When you perceive a moderate threat, you activate this system, preparing for fight or flight. Your energy levels increase, your senses sharpen, and you are ready to take action. This state is essential for self-preservation but can be overwhelming if prolonged.
The Bottom Rung: Immobilization (Dorsal Vagal Freeze)
At the very bottom of the ladder lies the state of immobilization, or freeze, controlled by your Dorsal Vagal Complex. This is your body’s ultimate survival strategy when fight or flight is not an option or has proven ineffective. It’s a primal, ancient response designed to minimize harm during inescapable threat.
Unpacking the Freeze Response
The freeze response is more than just being still. It’s a complex physiological and psychological shutdown, a complete system override designed to protect you when all other defenses fail.
The Biology of Freeze: A Last Resort
When you enter a freeze state, your body undergoes a remarkable transformation. Your heart rate and breathing slow dramatically, sometimes to dangerous levels. Your muscles may become flaccid or rigidly tensed, like a possum playing dead. Your metabolism plummets, conserving energy. You might experience a profound sense of numbness, both physical and emotional, as your body attempts to dissociate from the overwhelming experience. This is a survival mechanism that, while agonizing, can sometimes literally save your life by making you appear less threatening or by minimizing the pain of an inevitable attack.
Vasovagal Syncope
In extreme cases of freeze, you might experience vasovagal syncope, a temporary loss of consciousness due to a sudden drop in heart rate and blood pressure. This is an exaggerated dorsal vagal response, an involuntary fainting that further highlights the profound physiological shutdown associated with severe threat.
Psychological Manifestations of Freeze
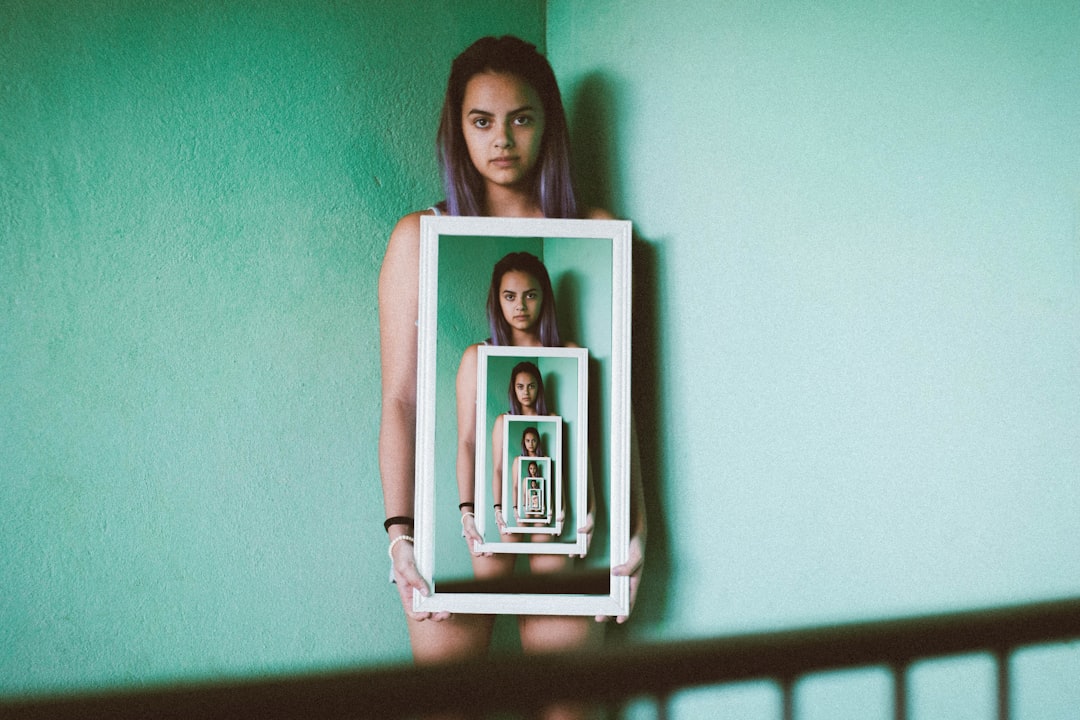
Beyond the physiological changes, the freeze response manifests significantly on a psychological level. You might experience a sense of detachment from your body, often described as an out-of-body experience. Time perception can become distorted, either slowing down or speeding up. Your cognitive functions may be severely impaired, making it difficult to think clearly, problem-solve, or even articulate your thoughts.
Dissociation: A Protective Veil
Dissociation is a hallmark of the freeze response. It’s as if your mind separates from your body, creating a psychological buffer against overwhelming pain or trauma. While this mechanism can offer temporary relief in dire circumstances, prolonged or habitual dissociation can hinder your ability to process experiences, engage with the present, and form meaningful connections.
“Playing Dead” Emotionally
Just as a creature physically plays dead, you might emotionally play dead during a freeze response. This can manifest as an inability to feel emotions, a sense of flat affect, or a complete shutdown of emotional expression. This emotional numbness, while protective in the moment, can contribute to feelings of emptiness and isolation later on.
Recognizing Freeze in Your Life

The freeze response isn’t always as dramatic as playing dead. It can manifest in subtle, everyday ways, often contributing to chronic stress, anxiety, and even depression. Understanding these more nuanced presentations is crucial for recognizing when you might be in a freeze state.
The “Deer in Headlights” Phenomenon
You’ve likely experienced or witnessed the classic “deer in headlights” response. Faced with a sudden, overwhelming situation, you may feel an inexplicable inability to move, speak, or even think. This is a common, albeit temporary, manifestation of the freeze response. You’re not consciously choosing to freeze; your ancient dorsal vagal system has taken the reins.
Chronic Immobilization and “Functional Freeze”
For individuals who have experienced prolonged or repeated trauma, the freeze response can become a habitual coping mechanism, leading to a state of “functional freeze.” You might appear to be going about your daily life, but internally, you are locked in a state of low-grade dorsal vagal activation.
Procrastination and Lack of Motivation
One common sign of functional freeze is chronic procrastination or a pervasive lack of motivation. You may have important tasks to complete, but you find yourself unable to start, feeling stuck or overwhelmed. This isn’t laziness; it’s your system signaling a perceived threat, leading to a shutdown of your ability to initiate action.
Social Withdrawal and Emotional Numbness
Functional freeze can also manifest as social withdrawal and emotional numbness. You might find it difficult to connect with others, struggling to express your feelings or even feel them. This can lead to feelings of isolation and a sense of being disconnected from the world around you.
Chronic Fatigue and Brain Fog
Persistent fatigue, even after adequate rest, and persistent “brain fog” – difficulty concentrating, remembering things, or thinking clearly – can also be indicators of a chronic freeze state. Your body is expending an immense amount of energy maintaining this shutdown, leaving little room for cognitive function or physical vitality.
Polyvagal theory provides a fascinating framework for understanding the freeze response, which is often overlooked in discussions about trauma and stress. For those interested in exploring this concept further, a related article can be found on Unplugged Psych, where the nuances of the freeze response are explained in detail. This resource offers valuable insights into how our nervous system reacts to perceived threats and can help individuals better understand their own responses to stress. You can read more about it in this informative piece here.
Navigating and Healing from Freeze
| Aspect | Description | Physiological Indicators | Behavioral Manifestations | Polyvagal Theory Explanation |
|---|---|---|---|---|
| Freeze Response | A state of immobilization or shutdown in response to extreme threat or overwhelm. | Decreased heart rate, reduced muscle tone, shallow breathing. | Stillness, lack of movement, dissociation, numbness. | Activation of the dorsal vagal complex leading to parasympathetic dominance and energy conservation. |
| Neural Pathway | Dorsal Vagal Complex (DVC) | Vagal nerve activity measured by heart rate variability (HRV) shows increased parasympathetic tone. | Reduced responsiveness to external stimuli. | DVC inhibits sympathetic nervous system, causing shutdown to protect the organism. |
| Triggering Factors | Perceived inescapable threat or overwhelming stress. | Elevated cortisol initially, then parasympathetic override. | Sudden cessation of movement or speech. | When fight or flight is not possible, freeze is a last-resort survival strategy. |
| Duration | Can last seconds to minutes, sometimes longer in trauma. | Prolonged low heart rate and low muscle activity. | Prolonged immobility, dissociative states. | Extended dorsal vagal activation can lead to shutdown and dissociation. |
| Recovery | Requires safe environment and social engagement. | Increase in heart rate variability and muscle tone. | Resumption of movement, speech, and social interaction. | Activation of ventral vagal complex promotes social engagement and regulation. |
While the freeze response is a powerful and ingrained survival mechanism, you are not condemned to live in perpetual shutdown. Understanding how to gently move out of freeze and cultivate a sense of safety is paramount for healing and well-being.
The Importance of Co-Regulation and Safety
One of the most crucial elements in moving out of a freeze state is establishing a sense of safety. Your ventral vagal system thrives on safety cues, both internal and external.
Safe and Sound Protocol (SSP)
Dr. Porges developed the Safe and Sound Protocol (SSP), a therapeutic intervention designed to retune your autonomic nervous system. The SSP involves listening to specially filtered music that emphasizes the frequencies of the human voice, which are processed by the same neural pathways as your ventral vagal system. This gentle auditory stimulation helps to strengthen your ventral vagal tone, enhancing your ability to feel safe and regulated.
Embodied Practices
Engaging in embodied practices can be incredibly powerful in shifting out of freeze. Practices that focus on grounding, bodily awareness, and gentle movement can help you reconnect with your physical body and begin to discharge trapped energy.
Somatic Experiencing (SE)
Somatic Experiencing, developed by Dr. Peter Levine, is a body-oriented therapeutic approach that helps individuals process and resolve trauma by gently guiding them to complete the natural “fight, flight, or freeze” responses that may have been interrupted during a traumatic event. By paying attention to bodily sensations, you can slowly release the energy that has been stored in your nervous system.
Gentle Movement and Pendulation
Engaging in gentle, mindful movement, such as walking, stretching, or yoga, can help to gradually bring your nervous system back online. The concept of “pendulation,” moving gently between states of activation and relaxation, can be particularly helpful in incrementally discharging trapped energy without overwhelming your system.
Cultivating Internal Resources
Alongside external support and embodied practices, developing internal resources is essential for building resilience against freeze.
Mindfulness and Self-Compassion
Practicing mindfulness can help you observe your internal states without judgment, allowing you to recognize when you are entering a freeze response. Combining this with self-compassion, treating yourself with kindness and understanding, is crucial for fostering a sense of safety and reducing the shame often associated with feeling “stuck.”
Breathwork
Conscious breathwork can be a powerful tool for regulating your nervous system. Slow, deep, diaphragmatic breathing activates your ventral vagal complex, signaling safety to your body and helping you shift out of a dorsal vagal state. Experiment with different breathing techniques, such as the 4-7-8 method, to find what resonates best with you.
Building a “Ventral Vagal Toolkit”
Create a personalized “toolkit” of resources and practices that help you feel safe and regulated. This might include listening to calming music, spending time in nature, connecting with supportive loved ones, engaging in creative activities, or anything else that brings you a sense of peace and presence.
The Journey Towards Regulation
Understanding the Polyvagal Theory’s freeze response empowers you to view your experiences through a new lens. It offers a framework for comprehending why you might feel stuck, numb, or overwhelmed, and, more importantly, provides pathways for healing and growth. Remember, you are not broken; your nervous system is simply employing an ancient and powerful survival strategy. By cultivating self-awareness, seeking supportive connections, and engaging in intentional practices, you can gently guide your system towards greater regulation, resilience, and a life of vibrant engagement. The journey out of freeze may be gradual, but with patience and perseverance, you can learn to navigate the intricate landscape of your autonomic nervous system and reclaim a sense of safety and vitality in your life.
WARNING: Your “Peace” Is Actually A Trauma Response
FAQs
What is the polyvagal theory?
The polyvagal theory, developed by Dr. Stephen Porges, explains how the autonomic nervous system regulates our physiological state in response to stress and safety cues. It highlights the role of the vagus nerve in controlling heart rate, social engagement, and defensive behaviors such as fight, flight, or freeze.
What does the freeze response mean in the context of polyvagal theory?
In polyvagal theory, the freeze response is a state of immobilization triggered by the dorsal vagal complex, a branch of the vagus nerve. It is a survival mechanism activated when fight or flight responses are not possible, leading to a shutdown or dissociation to protect the individual from perceived life-threatening situations.
How does the freeze response differ from fight or flight?
Fight or flight responses are activated by the sympathetic nervous system and prepare the body to confront or escape danger. The freeze response, however, is mediated by the parasympathetic nervous system via the dorsal vagal pathway, resulting in decreased heart rate, reduced movement, and a state of immobilization or dissociation.
Can the freeze response be consciously controlled or managed?
While the freeze response is an automatic physiological reaction, individuals can learn to recognize and manage it through therapeutic techniques such as mindfulness, somatic experiencing, and polyvagal-informed therapy. These approaches help regulate the nervous system and promote a return to a state of safety and social engagement.
Why is understanding the freeze response important for mental health?
Understanding the freeze response helps clinicians and individuals recognize how trauma and stress impact the nervous system. It provides insight into symptoms like dissociation, numbness, or shutdown, enabling more effective treatment strategies that address underlying physiological states rather than just psychological symptoms.




